Delayed presentation of SC fractures – Open Reduce now or accept for Future Osteotomy
Vol 1 | Issue 1 | July-Sep 2015 | page:23-25 | Premal Naik, Hitesh Chauhan.
Authors : Premal Naik[1*], Hitesh Chauhan[1].
[1] Rainbow Superspeciality hospital & Children’s Orthopaedic Centre, Ahmedabad, Gujarat, India.
Address of Correspondence
Dr Premal Naik
Rainbow Superspeciality hospital & Children’s Orthopaedic Centre, Ahmedabad, Gujarat, India.
Email: premalnaik@gmail.com
Abstract
Background: Delayed presentations of paediatric supracondylar humerus fractures presents a unique situation. The decision between conservative management, closed reduction and fixation and open reduction are to be weighed against malunion and correction at later date. The existing literature talks about delay in terms of hours or days, however we in our country see patients presenting weeks later after injury. There are no clear existing guidelines for such delayed presentation and decision making is multifactorial depending on age, amount of displacement, degree of union and days of delay. In this review we have presented the various available treatment modality and a treatment algorithm for management of delayed presentation of paediatric supracondylar humerus fracture.
Keywords: Supracondylar Humerus fracture, delayed presentation, management.
Introduction
In our practice we still encounter patients with supracondylar fracture of distal Humerus presenting late, though recently the number is drastically reducing. Late presentation is considered when there is delay in presentation of more than 2 days after injury[1, 2]. The reasons of delay could be due to lack of awareness and initial treatment by bone-setters, injury in areas remote from health facilities. Sometimes primary centers (not well equipped) tend to shift patients with excessive swelling and associated neurovascular problems to higher centers leading to further delay in final treatment. Treatment of late cases has higher chances of perioperative and postoperative complications like iatrogenic nerve injury, Volkmann’s ischemic contracture, cubitus varus, elbow stiffness and myositis ossificans [3-5]. There remains a dilemma while managing late cases, whether to treat it as fresh supracondylar fracture or to allow it to mal-unite and consider for corrective surgery at later stage. Unfortunately in literature there are no clear guide lines or consensus regarding management of delayed presentation of supracondylar fractures.
Literature review
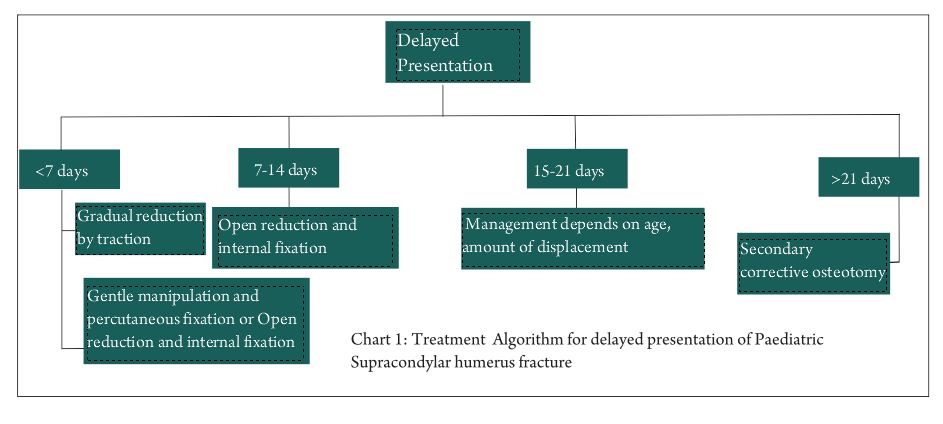
In delayed presentation cases up to 2 weeks we can adopt one of the following treatment modalities
1. Gradual reduction of fracture with traction (skin traction or skeletal)
2. Skeletal traction followed by percutaneous fixation
3. Trial of gentle manipulation and percutaneous fixation
4. Open reduction and internal fixation
In cases presenting three weeks after injury gradual reduction with traction is mostly not helpful. In such cases open reduction becomes technically difficulty because of difficulty in delineating uniting fracture fragments and need for greater soft tissue dissection. Hence it is imperative to allow fracture to unite and perform secondary corrective osteotomy at later stage (if required) after remodeling stage. Devnani et. al [6] in their series of 28 children with average delay in presentation of 5.6 days (2 to 21 days) advocated gradual fracture reduction with traction. Average hospital stay for treatment was 14 days (12 – 18 days) and 71% patients had good results according to Flynn criteria [7]. No patient had treatment related neurological injuries or new bone formation. They observed that overall functional outcome was better in patients presenting within 7 days of injury.
Agus et al [8] reported 13 patients with delay of more than 1 day and extensive swelling. Patients were treated with skeletal traction till satisfactory healing of skin and soft tissue, followed by percutaneous pinning. In his series average hospitalization was 7 days, 85% patient had excellent functional outcome and 77% had excellent cosmetic outcome. Tiwari et al [9] in their series of 40 patients presenting within 7 days, could successfully reduce 25 fractures by gentle closed manipulation under image intensifier and stabilize percutaneously. They advocated open reduction using mediolateral (posterior triceps sparing) approach in patients presenting after 7 days. Lal and Bhan [10] in their series of 20 patients with a delay of 11 – 17 days , performed open reduction by posterior approach after primary immobilization in Thomas splint and healing of skin and soft tissue oedema. They performed V-Y plasty of triceps in all cases for improvement of flexion. All patients had unsatisfactory functional recovery according Mitchell’s and Adam’s criteria [11]. In their series 35% patients had cubitus varus deformity and 85 % patient developed myositis ossificans. Abdullah Eren[12] in their series of 31 patient with an average delay of 6 days (2- 19 days) performed open reduction by medial approach and cross K-wire fixation. All patients had full functional recovery at 5 months. They reported 6.5% pin tract infection and 22.5 % of cubitus varus. Tahir et al [13] performed open reduction by Kocher’s incision in 40 patients with an average delay of 5 days. List of complication in this series included myositis ossificans and restricted elbow movements in 5% and pin tract infection in 6.5 %. Most of patients (95%) achieved full range of motion.
Yildirim et al [14] in their prospective study of 190 patients on timing of surgical treatment of type III supracondylar humerus fracture showed that open surgery was inevitable after a delay of 32 hours after injury.
Discussion
Surgeons tend to choose modalities of treatment depending on expertise level, type of set up and patient factors (time of presentation, amount of swelling, neurovascular injury, ipsilateral injury).
Conservative treatment:This modality would be considered when resources are not adequate or patient condition precludes more aggressive treatment. One can choose between skin traction and skeletal traction to maintain reduction. For skeletal traction pin is passed through the olecranon.
Advantages of gradual reduction by traction
1.Traction allows simultaneous healing of soft tissues along with reduction of fracture
2. Chances of iatrogenic neurovascular injury are remote
3. Many authors have reported Incidence of cubitus varus to be comparable to other method with traction [6, 15]
4.Technically easy and can be performed at small centers
Disadvantages of gradual reduction 1. Prolonged hospital stay with cumbersome nursing care
2. Patient presenting late (more than 7 days) tend to have inferior results [6]
Operative treatment: In fully equipped set up with good patient parameters and experienced surgical team, operative treatment is commonly chosen.
Advantages of open reduction and internal fixation are:-
1. Accurate reduction, appropriate fixation and early mobilization
2. Lesser hospital stay
Disadvantages are –
1. Technically demanding procedure and requires experienced surgeon
2. Higher chances of myositis ossificans due to soft tissue stripping and iatrogenic nerve injury.
Authors preferred treatment
In patients presenting within 2 weeks and if skin condition permits, we prefer trial of gentle manipulation and reduction under anesthesia. If satisfactory reduction is achieved then fracture is stabilized with percutaneous K wire fixation (Illustrative case 1).
At the same stage if satisfactorily reduction is not achieved, we proceed for open reduction. We use anteromedial or anterolateral approach depending on direction prominent spike of proximal fragment (if proximal fragment has medial spike we use anteromedial approach and with lateral spike anteriolateral) (Case 2).
We prefer shortening of proximal fragment to achieve easy and accurate reduction over performing extensive soft tissue dissection.
In patients presenting after 3 weeks we prefer to accept union in malposition and consider for corrective osteotomy at later date.
Illustrative cases
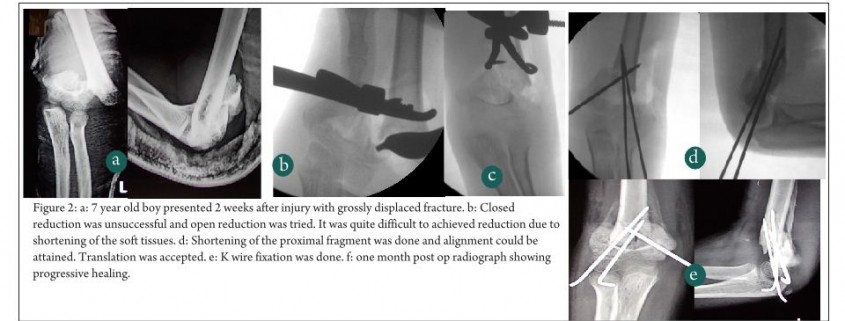
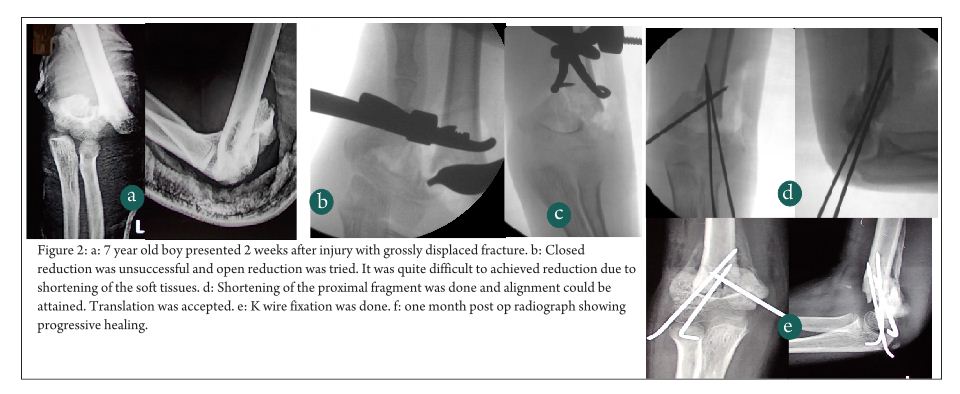
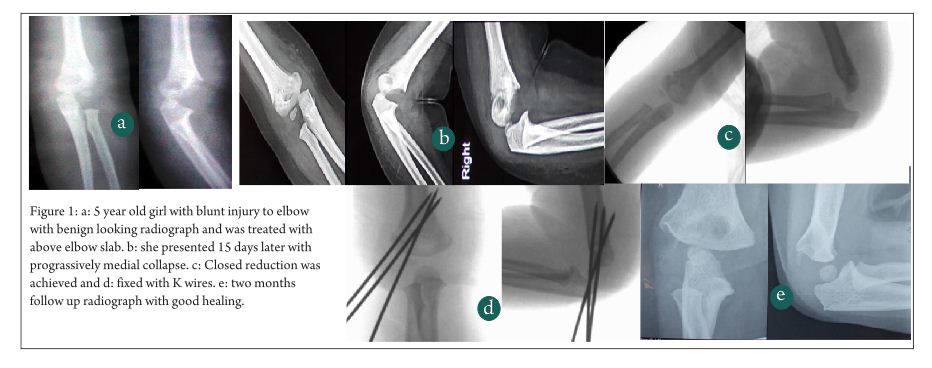
Case 1:- 1 year old female, sustained injury in right arm while playing. Primarily she was treated conservatively with above elbow slab (Fig. 1). She presented to us 15 days post injury, with progressive medial collapse Successful reduction was obtained after gentle manipulation under anaesthesia and fixation was done with lateral wires.
Case 2 – 7 year, Male with RTA, sustained injury in left upper limb which was primarily treated elsewhere with above elbow slab. He presented to us two weeks after injury. He had ipsilateral distal radial physeal injury and type 3 supracondylar fracture (Fig. 2). After failed gentle attempt of closed reduction, open reduction was planned by anterolateral approach (as proximal spike was protruding laterally). Due to severe soft tissue contracture reduction of fracture was not possible as length could not be achieved. Instead of aggressive soft tissue dissection, shortening of proximal fragment was performed, translation was accepted and fracture was fixed with K wires.
References
1. Sankar WN, Hebela NM, Skaggs DL, Flynn JM. Loss of pin fixation in displaced supracondylar humeral fractures in children: causes and prevention. The Journal of Bone & Joint Surgery. 2007;89(4):713-7.
2. Shannon FJ, Mohan P, Chacko J, D’Souza LG. “Dorgan’s” percutaneous lateral cross-wiring of supracondylar fractures of the humerus in children. Journal of Pediatric Orthopaedics. 2004;24(4):376-9.
3. Campbell WC, Preston RL. Operative Orthopaedic. Annals of Surgery. 1939;110(4):800.
4. Harris I. Supracondylar fractures of the humerus in children. Orthopedics. 1992;15(7):811-7
5. Minkowitz B, Busch MT. Supracondylar humerus fractures. Current trends and controversies. The Orthopedic clinics of North America. 1994;25(4):581-94.
6. Devnani A. Late presentation of supracondylar fracture of the humerus in children. Clinical orthopaedics and related research. 2005;431:36-41.
7. Flynn JC, Matthews JG, Benoit RL. Blind pinning of displaced supracondylar fractures of the humerus in children. The Journal of Bone & Joint Surgery. 1974;56(2):263-72.
8. Agus H, Kalenderer Ö, Kayal C, Eryanlmaz G. Skeletal traction and delayed percutaneous fixation of complicated supracondylar humerus fractures due to delayed or unsuccessful reductions and extensive swelling in children. Journal of Pediatric Orthopaedics B. 2002;11(2):150-4.
9. Tiwari A, Kanojia R, Kapoor S. Surgical management for late presentation of supracondylar humeral fracture in children. Journal of Orthopaedic Surgery. 2007;15(2).
10. Lal G, Bhan S. Delayed open reduction for supracondylar fractures of the humerus. International orthopaedics. 1991;15(3):189-91.
11. Mitchell WJ, Adams JP. Supracondylar fractures of the humerus in children: a ten-year review. JAMA. 1961;175(7):573-7.
12. Eren A, Güven M, Erol B, Cakar M. Delayed surgical treatment of supracondylar humerus fractures in children using a medial approach. Journal of children’s orthopaedics. 2008;2(1):21-7.
13. Tahir A, Majid F, Ali MN, Qureshi MA. Treatment of Old Supracondylar Fractures of Humerus In Children. Journal of Surgery Pakistan (International). 2012;17:4.
14. Yildirim AO, Unal VS, Oken OF, Gulcek M, Ozsular M, Ucaner A. Timing of surgical treatment for type III supracondylar humerus fractures in pediatric patients. Journal of children’s orthopaedics. 2009;3(4):265-9.
15. Piggot J, Graham H, McCoy G. Supracondylar fractures of the humerus in children. Treatment by straight lateral traction. Journal of Bone & Joint Surgery, British Volume. 1986;68(4):577-83
.
| How to Cite this Article: Naik P, Chauhan H. Delayed presentation of SC fractures – Open Reduce now or Accept for Future Osteotomy. International Journal of Paediatric Orthopaedics July-Sep 2015;1(1):23-25. |