License
International Journal of Paediatric Orthopaedics is licensed under a
https://creativecommons.org/licenses/by-nc-sa/4.0/
Publisher
Official Journal of:
Paediatric Orthopaedic Society of India (POSI)
Publisher:
ResearchOne Publishing House,
An "Indian Orthopaedic Research Group (IORG) initiative.
IORG House,
A-203, Manthan Apts, Shreesh CHS, Hajuri Road,
Thane [West], Maharashtra, India.
Pin Code- 400604
Tel- 02225834545
Publisher Email: indian.ortho@gmail.com
Editor Email: editor.ijpo@gmail.com
pwktoto
holyslot123
Amanah99
Rupiah777
horastogel
cuanslot
okta138
tango168
lotus777
bostoto138
medali69
milojitu
Lotre78
lux77
Gorilatoto
Hoki338
Dewapoker77
baikbet
sule78
lavatoto
uang138
Merak99
porto4d
hemattoto
Kaca138
puri138
anginbet
Joglo4d
juragantogel
Mahyong69
sojubet
sakti777
StarJoker69
grab78
spacetogel
jarum169
Kudatoto
pangkalanbet
ten88
opera99
satelit69
koin88
pondok338
jaring338
pubtogel
milo338
thor388
deltatoto
bdjitu
mirana99
amat123
autobet123
Shio77
gemoy188
planet888
Maria99
makmurwin
pakdejp
geber777
lato777
Melatibet
bankslot
hujantogel
coco69
Rusa69
Apollo303
sule777
namabet
Mars77
moon138
Pancingslot
Pulaubet
rumah88
cumi303
prada68
versace138
Koala4d
lobby69
lux78
usaha4d
kambingtogel
Musangtoto
delta777
Jeweltoto
pos188
lava77
maluku303
kompor88
luckslot
Lotre169
lotus68
raffi169
tambang388
ratuzeusqq
dinasti99
Modalhoki108
asiajitu
judi78
astra78
partaiqq
rumah69
Meriam123
evosbet88
Sayangbet
Lilin4d
Cemaraslot
furla69
kumis4d
Bandungslot
japan78
hokislot123
hulk303
Pragmatic69
chivas69
krisna188
Lyonslot
ASIABET168
topislot
bola123
ultra365
ios55
kompor77
sinaga138
kelapabet
padang777
Rajawin777
Jakarta88slot
Becak168
babetogel
primaslot
Moonslot
palu338
pulautogel
botaktogel
platinum138
cici169
gunturtogel
Kacang4d
dewabet138
spin388
homebet69
bursatoto
mami4d
pasbet
aduhoki
lava69
pagoda388
meledak99
dalang138
Gama188
dino777
papua338
darat123
hokiwin55
Cobra777
Merak88
crown78
preman77
grab188
terminal388
apiwin
madura78
sinar303
Dupawin
Santuy188
kera388
Modalhoki68
omuslot
Peri123
divabet
macau388
Angsa138
keris69
DOMINOPKV
Bos69
Sawitjitu
jaring99
layar77
tayototo
taro168
pejuang388
next88
harapan168
hemat123
Shio88
apidewa77
parisjp
pohon69
Lotre777
taruna123
asean168
giga69
StarJoker123
tempat99
Sisir4d
Tokek78
bosstogel
pakdeslot88
wisslot
rumah108
dominoslot
cola123
jili88
kompas77
bisnis77
kungfu69
Arjuna77
sensa123
Piramida4d
gacor365
pucuk777
Lotre123
wayang777
Gama178
WLA88
langitmpo
Robot4d
kumbang123
Logam4d
Sawit138
Bca168
petir88
tokyobet
tempo123
Permen178
Gacorbos99
wiratogel
LUNAS805
sateslot
barbar188
maxwin123
pecahtogel
Menang77
demotogel
trisula4d
candy138
bostoto188
demo388
citatogel
SIRKUIT138
Boy4d
Kalaslot
formulabet
Kode99
icon55
domino123
cartel303
jingga4d
Luxuryqq
space168
Legenda4d
porto169
api69
ASIAMPO77
wiki69
fasslot
cincin77
rajatoto68
Merak78
batastogel
gem108
buku99
furlabet
versace168
Sayang777
marvel365
kumis138
sushitoto
cbototo
latar77
Hadiah4d
solusi138
udara4d
sayang188
maha777
milo55
taro303
Dunia88
sejuta188
Dewapokertogel
Luxurygg
KOBOYPOKER
Aksara77
amat303
unggul123
oris77
kingdomjitu
merci4d
Aontoto
gemoyslot
geloratoto
layar69
winning138
sobet78
klik303
gilagg
bantamtoto
Sbo4d
Tombol4d
maya303
spin6d
sumo123
lambe88
barbar88
kadobet168
solid169
oasis365
karo303
duta69
sumo88
Pandawa123
ipar777
bengkelslot
macanslot
abc69
judolbetqq
Laku123
obor77
Lampion4d
memori77
jepang169
plntoto
ASIAPKV
Duyung88
Hijau123
dewanslot
MAXWIN888
SUARABET77
empirebet
Kucingtoto
kakek138
idr188
coca123
sisri77
jamu123
cumi99
fire123
persentogel
moon4d
dutabet
jaring365
Bigwin178
Gacorbos169
toto388
evosgamingg
kado99
WLA55
kadal303
rumah168
Poker138
Aztectoto
gasing78
extrabet
urban168
Topengslot
planet388
Angkatoto77
mulia88
qq69
luck388
epictogel
GACORBOS
icon169
atlas169
bentototo
jamu4d
libas169
holiday69
hulk77
skor77
karo168
colekbet
Bendera99
suhu4d
Dayak123
radentogel
KOBOY888
memori108
lajubet888
JUARAWIN88
BIMO77
jokerbetqq
AREASLOTO
juara77
dewi138
DEWIBET777
nusapoker
jilibet
Ikan303
kadalslot
depototo
harum123
pawang88
krisna123
madu55
Khusustogel
taktik388
Wahana4d
ovo168
mesinslot
Gogo90
bromo99
Badutjitu
Mega777
sentosa69
kamus168
Tigerslot
tempatslot
wazebet
sekai777
airtogel
Agen99
colek777
pasang388
pigi388
Angkatoto123
batam69
kudetabet69
mewah123
fuji338
papua78
murahpoker
cincin365
memori69
hantu78
anak777
Kapten99
Nanas188
Glory77
wiki78
PEDANGBET
mahjongs138
ipar78
motoslot88
POV99
bingo4d
ratuslot777
YUPI188
ASIASLOT888
fire777
pasti138
batam777
julietslot
iklan88
kamus77
sobet99
capital99
Sicbo4d
paris4d
daya365
amat168
roslot55
Kaktusslot
cakra123
Abu123
krisna77
guntur365
PEDANGJITU
panca123
Kodok123
ASIAKING777
JPSLOT168
wuling88
kaya77
KOBOIBOLA
garpu777
kingbet169
pir69
extra188
oren77
cair365
kingdomjp
dewaslot138
nagapoker777
cici138
Daun777
surga6d
holyslottoto
jakarta303
dinasti777
suara78
Mbah4d
HOKIOM88
zona77
unggul169
tempat123
Arus138
retro388
mampirtoto
sulaptogel
nagawin168
pecah188
bangsa338
ASIAHOKI88
neopoker
mesin188
canduslot777
dino78
asus88
Mangga4d
kumistogel
nama88
kkslot55
LUNA999
Tokcer69
Logam303
kkslot108
lgo188
gemoy777
ultra99
tahunslot
ligajp88
kampusslot
babe69
macau128
taktik123
kado338
Angsa77
latarslot
juliet777
lavaslot
suburbet
doyan77
ladang77
Dupaslot
YUPIBET
AREA188
betagg
usaha169
AREAWIN88
megawinbet
Tokcer168
mandiri99
MANTAP138
mahal99
Gobertogel
abc77
mulia99
bonus303
kembar388
sensatogel
atom188
gebyar77
baik388
balon138
Master77
ovo338
gaco169
edanbet
pistolslot
air169
kembang169
dna303
wigo123
ladangslot
pasang338
suryatogel
DOMINOBET77
kembar188
diva388
pohonjitu
Sakuraqq
kumis168
ASIATOTO777
Premium188
rupiah4d
CERIAPOKER
KAYA78
kebunbet
sawi69
pub365
pesiar69
Wild777
Tores777
paus168
bom108
Dollarjitu
vegas77
wis338
Kancil69
angkasaslot
Dolan138
semangat303
jaritogel
daun69
nova123
darat303
SERUBET88
selat123
hantu88
serbatoto
balon123
tenbet
padi78
benuawin
Sensa188
Emas88
Rajawalitogel
musangtogel
sarana78
sugar365
lexus108
bom123
kso123
luck4d
puncak88
vista123
muara69
Rutantoto
ceria88
RAFI777
alasbet
durentoto
mpomaster
cipitbet
usaha138
leobet
mantra168
Akun188
Nanastogel
alexa88
Tombol168
slotbom68
solid78
gunturslot
sake138
Gloryslot
luck77
raksasa138
mildbet
Doku123
Yakuza777
bostoto77
jutawan168
odin123
lampu168
cumi168
mega169
puri188
petatogel
dadu168
mahadewa168
karirtogel
istana88
serbu123
kumbang99
pulau169
Sarangslot88
muliaslot
tiktoktoto
retro4d
ayo68
Dugem88
jepe338
bns99
leo303
turbo77
timur77
baiktogel
masterbet123
Mansionslot
petirslot
retro69
unggul168
POV69
musik168
kapaljudi777
Habanero138
marvel188
kejubet
ios99
Ninjaslot
permen169
fix338
koi138
madura168
gerbang338
desa77
sushi168
Ikanslot
opera123
oren365
luckbet
Rusa77
Ungu77
hugo99
medan123
zodiaktoto
papua168
mansion88
luck99
asean188
rajazeus138
seru78
kampung99
Target99
gas123
coca4d
dinastibet
sultanbet188
Alamtoto
pwktoto pwktoto
rajagaming-52
rajagaming-53
rajagaming-54
rajagaming-55
rajagaming-56
rajagaming-57
rajagaming-58
rajagaming-59
rajagaming-6
rajagaming-60
rajagaming-61
rajagaming-62
rajagaming-63
rajagaming-64
rajagaming-65
rajagaming-66
rajagaming-67
rajagaming-68
rajagaming-69
rajagaming-7
rajagaming-70
rajagaming-71
rajagaming-72
rajagaming-73
rajagaming-74
rajagaming-75
rajagaming-76
rajagaming-77
rajagaming-78
rajagaming-79
rajagaming-8
rajagaming-80
rajagaming-81
rajagaming-82
rajagaming-83
rajagaming-84
rajagaming-85
rajagaming-86
rajagaming-87
rajagaming-88
rajagaming-89
rajagaming-9
rajagaming-90
rajagaming-91
rajagaming-92
rajagaming-93
rajagaming-94
rajagaming-95
rajagaming-96
rajagaming-97
rajagaming-98
rajagaming-99
sibayak99
triadtotogroup
nagatoto88
garwa4d
Kirintoto
triadsgp
triadsyd
triadjitu
triadmacau
triadtoto
triadtogel
triad4d
triadhk
torpedo99
scatter99
boom138
bosslot138
sibayak99
emas69
triad303
triadslot
pwktoto
triadtogel
triadhk
nagatoto88
garwa4d
torpedo4d
triadmacau
triadtoto
triadmacau
triadtoto
triadtogel
triadhk
scatter99
sibayak99
emas69
triadjitu
emas69
scatter99
sibayak99
boom138
pwktoto
torpedo4d
torpedo4d
torpedo4d
torpedo4d
nagatoto88
nagatoto88
nagatoto88
garwa4d
garwa4d
garwa4d
triadtoto
triadtoto
triadtoto
triadtogel
triadtogel
triadtogel
triad4d
triad4d
triad4d
triad4d
triad4d
triad4d
triadhk
triadhk
triadhk
triadhk
triadhk
triadhk
triadmacau
triadmacau
triadjitu
triadjitu
triadjitu
scatter99
scatter99
scatter99
scatter99
scatter99
sibayak99
sibayak99
sibayak99
sibayak99
sibayak99
sibayak99
sibayak99
sibayak99
boom138
emas69
emas69
rokettoto
rokettoto
rokettoto
rokettoto
bukitdita
kirintoto
kirintoto
triadsgp
triadsgp
triadsyd
triadsyd
torpedo99
torpedo99
torpedo99
torpedo99
premium138
premium138
premium138
premium138
premium138
premium138
bosslot138
bosslot138
bosslot
bosslot138
bosslot138
pusat69
pusat69
dompet69
dompet69
dompet69
dompet138
dompet188
dompet168
dompet123
harta69
triadslot
triadslot
triad303
138vip
138vip
triadtogel
triadtoto
triad4d
triadhk
triadhk
triad4d
triadtogel
triadjitu
triadmacau
boom138
garwa4d
scatter99
emas69
torpedo4d
nagatoto88
vinaslot
vinaslot
vinaslot
pwktoto
holyslot123
Amanah99
Rupiah777
horastogel
cuanslot
okta138
tango168
lotus777
bostoto138
medali69
milojitu
Lotre78
lux77
Gorilatoto
Hoki338
Dewapoker77
baikbet
sule78
lavatoto
uang138
Merak99
porto4d
hemattoto
Kaca138
puri138
anginbet
Joglo4d
juragantogel
Mahyong69
sojubet
sakti777
StarJoker69
grab78
spacetogel
jarum169
Kudatoto
pangkalanbet
ten88
opera99
satelit69
koin88
pondok338
jaring338
pubtogel
milo338
thor388
deltatoto
bdjitu
mirana99
amat123
autobet123
Shio77
gemoy188
planet888
Maria99
makmurwin
pakdejp
geber777
lato777
Melatibet
bankslot
hujantogel
coco69
Rusa69
Apollo303
sule777
namabet
Mars77
moon138
Pancingslot
Pulaubet
rumah88
cumi303
prada68
versace138
Koala4d
lobby69
lux78
usaha4d
kambingtogel
Musangtoto
delta777
Jeweltoto
pos188
lava77
maluku303
kompor88
luckslot
Lotre169
lotus68
raffi169
tambang388
ratuzeusqq
dinasti99
Modalhoki108
asiajitu
judi78
astra78
partaiqq
rumah69
Meriam123
evosbet88
Sayangbet
Lilin4d
Cemaraslot
furla69
kumis4d
Bandungslot
japan78
hokislot123
hulk303
Pragmatic69
chivas69
krisna188
Lyonslot
ASIABET168
topislot
bola123
ultra365
ios55
kompor77
sinaga138
kelapabet
padang777
Rajawin777
Jakarta88slot
Becak168
babetogel
primaslot
Moonslot
palu338
pulautogel
botaktogel
platinum138
cici169
gunturtogel
Kacang4d
dewabet138
spin388
homebet69
bursatoto
mami4d
pasbet
aduhoki
lava69
pagoda388
meledak99
dalang138
Gama188
dino777
papua338
darat123
hokiwin55
Cobra777
Merak88
crown78
preman77
grab188
terminal388
apiwin
madura78
sinar303
Dupawin
Santuy188
kera388
Modalhoki68
omuslot
Peri123
divabet
macau388
Angsa138
keris69
DOMINOPKV
Bos69
Sawitjitu
jaring99
layar77
tayototo
taro168
pejuang388
next88
harapan168
hemat123
Shio88
apidewa77
parisjp
pohon69
Lotre777
taruna123
asean168
giga69
StarJoker123
tempat99
Sisir4d
Tokek78
bosstogel
pakdeslot88
wisslot
rumah108
dominoslot
cola123
jili88
kompas77
bisnis77
kungfu69
Arjuna77
sensa123
Piramida4d
gacor365
pucuk777
Lotre123
wayang777
Gama178
WLA88
langitmpo
Robot4d
kumbang123
Logam4d
Sawit138
Bca168
petir88
tokyobet
tempo123
Permen178
Gacorbos99
wiratogel
LUNAS805
sateslot
barbar188
maxwin123
pecahtogel
Menang77
demotogel
trisula4d
candy138
bostoto188
demo388
citatogel
SIRKUIT138
Boy4d
Kalaslot
formulabet
Kode99
icon55
domino123
cartel303
jingga4d
Luxuryqq
space168
Legenda4d
porto169
api69
ASIAMPO77
wiki69
fasslot
cincin77
rajatoto68
Merak78
batastogel
gem108
buku99
furlabet
versace168
Sayang777
marvel365
kumis138
sushitoto
cbototo
latar77
Hadiah4d
solusi138
udara4d
sayang188
maha777
milo55
taro303
Dunia88
sejuta188
Dewapokertogel
Luxurygg
KOBOYPOKER
Aksara77
amat303
unggul123
oris77
kingdomjitu
merci4d
Aontoto
gemoyslot
geloratoto
layar69
winning138
sobet78
klik303
gilagg
bantamtoto
Sbo4d
Tombol4d
maya303
spin6d
sumo123
lambe88
barbar88
kadobet168
solid169
oasis365
karo303
duta69
sumo88
Pandawa123
ipar777
bengkelslot
macanslot
abc69
judolbetqq
Laku123
obor77
Lampion4d
memori77
jepang169
plntoto
ASIAPKV
Duyung88
Hijau123
dewanslot
MAXWIN888
SUARABET77
empirebet
Kucingtoto
kakek138
idr188
coca123
sisri77
jamu123
cumi99
fire123
persentogel
moon4d
dutabet
jaring365
Bigwin178
Gacorbos169
toto388
evosgamingg
kado99
WLA55
kadal303
rumah168
Poker138
Aztectoto
gasing78
extrabet
urban168
Topengslot
planet388
Angkatoto77
mulia88
qq69
luck388
epictogel
GACORBOS
icon169
atlas169
bentototo
jamu4d
libas169
holiday69
hulk77
skor77
karo168
colekbet
Bendera99
suhu4d
Dayak123
radentogel
KOBOY888
memori108
lajubet888
JUARAWIN88
BIMO77
jokerbetqq
AREASLOTO
juara77
dewi138
DEWIBET777
nusapoker
jilibet
Ikan303
kadalslot
depototo
harum123
pawang88
krisna123
madu55
Khusustogel
taktik388
Wahana4d
ovo168
mesinslot
Gogo90
bromo99
Badutjitu
Mega777
sentosa69
kamus168
Tigerslot
tempatslot
wazebet
sekai777
airtogel
Agen99
colek777
pasang388
pigi388
Angkatoto123
batam69
kudetabet69
mewah123
fuji338
papua78
murahpoker
cincin365
memori69
hantu78
anak777
Kapten99
Nanas188
Glory77
wiki78
PEDANGBET
mahjongs138
ipar78
motoslot88
POV99
bingo4d
ratuslot777
YUPI188
ASIASLOT888
fire777
pasti138
batam777
julietslot
iklan88
kamus77
sobet99
capital99
Sicbo4d
paris4d
daya365
amat168
roslot55
Kaktusslot
cakra123
Abu123
krisna77
guntur365
PEDANGJITU
panca123
Kodok123
ASIAKING777
JPSLOT168
wuling88
kaya77
KOBOIBOLA
garpu777
kingbet169
pir69
extra188
oren77
cair365
kingdomjp
dewaslot138
nagapoker777
cici138
Daun777
surga6d
holyslottoto
jakarta303
dinasti777
suara78
Mbah4d
HOKIOM88
zona77
unggul169
tempat123
Arus138
retro388
mampirtoto
sulaptogel
nagawin168
pecah188
bangsa338
ASIAHOKI88
neopoker
mesin188
canduslot777
dino78
asus88
Mangga4d
kumistogel
nama88
kkslot55
LUNA999
Tokcer69
Logam303
kkslot108
lgo188
gemoy777
ultra99
tahunslot
ligajp88
kampusslot
babe69
macau128
taktik123
kado338
Angsa77
latarslot
juliet777
lavaslot
suburbet
doyan77
ladang77
Dupaslot
YUPIBET
AREA188
betagg
usaha169
AREAWIN88
megawinbet
Tokcer168
mandiri99
MANTAP138
mahal99
Gobertogel
abc77
mulia99
bonus303
kembar388
sensatogel
atom188
gebyar77
baik388
balon138
Master77
ovo338
gaco169
edanbet
pistolslot
air169
kembang169
dna303
wigo123
ladangslot
pasang338
suryatogel
DOMINOBET77
kembar188
diva388
pohonjitu
Sakuraqq
kumis168
ASIATOTO777
Premium188
rupiah4d
CERIAPOKER
KAYA78
kebunbet
sawi69
pub365
pesiar69
Wild777
Tores777
paus168
bom108
Dollarjitu
vegas77
wis338
Kancil69
angkasaslot
Dolan138
semangat303
jaritogel
daun69
nova123
darat303
SERUBET88
selat123
hantu88
serbatoto
balon123
tenbet
padi78
benuawin
Sensa188
Emas88
Rajawalitogel
musangtogel
sarana78
sugar365
lexus108
bom123
kso123
luck4d
puncak88
vista123
muara69
Rutantoto
ceria88
RAFI777
alasbet
durentoto
mpomaster
cipitbet
usaha138
leobet
mantra168
Akun188
Nanastogel
alexa88
Tombol168
slotbom68
solid78
gunturslot
sake138
Gloryslot
luck77
raksasa138
mildbet
Doku123
Yakuza777
bostoto77
jutawan168
odin123
lampu168
cumi168
mega169
puri188
petatogel
dadu168
mahadewa168
karirtogel
istana88
serbu123
kumbang99
pulau169
Sarangslot88
muliaslot
tiktoktoto
retro4d
ayo68
Dugem88
jepe338
bns99
leo303
turbo77
timur77
baiktogel
masterbet123
Mansionslot
petirslot
retro69
unggul168
POV69
musik168
kapaljudi777
Habanero138
marvel188
kejubet
ios99
Ninjaslot
permen169
fix338
koi138
madura168
gerbang338
desa77
sushi168
Ikanslot
opera123
oren365
luckbet
Rusa77
Ungu77
hugo99
medan123
zodiaktoto
papua168
mansion88
luck99
asean188
rajazeus138
seru78
kampung99
Target99
gas123
coca4d
dinastibet
sultanbet188
Alamtoto
pwktoto pwktoto
rajagaming-52
rajagaming-53
rajagaming-54
rajagaming-55
rajagaming-56
rajagaming-57
rajagaming-58
rajagaming-59
rajagaming-6
rajagaming-60
rajagaming-61
rajagaming-62
rajagaming-63
rajagaming-64
rajagaming-65
rajagaming-66
rajagaming-67
rajagaming-68
rajagaming-69
rajagaming-7
rajagaming-70
rajagaming-71
rajagaming-72
rajagaming-73
rajagaming-74
rajagaming-75
rajagaming-76
rajagaming-77
rajagaming-78
rajagaming-79
rajagaming-8
rajagaming-80
rajagaming-81
rajagaming-82
rajagaming-83
rajagaming-84
rajagaming-85
rajagaming-86
rajagaming-87
rajagaming-88
rajagaming-89
rajagaming-9
rajagaming-90
rajagaming-91
rajagaming-92
rajagaming-93
rajagaming-94
rajagaming-95
rajagaming-96
rajagaming-97
rajagaming-98
rajagaming-99
sibayak99
triadtotogroup
nagatoto88
garwa4d
Kirintoto
triadsgp
triadsyd
triadjitu
triadmacau
triadtoto
triadtogel
triad4d
triadhk
torpedo99
scatter99
boom138
bosslot138
sibayak99
emas69
triad303
triadslot
pwktoto
triadtogel
triadhk
nagatoto88
garwa4d
torpedo4d
triadmacau
triadtoto
triadmacau
triadtoto
triadtogel
triadhk
scatter99
sibayak99
emas69
triadjitu
emas69
scatter99
sibayak99
boom138
pwktoto
torpedo4d
torpedo4d
torpedo4d
torpedo4d
nagatoto88
nagatoto88
nagatoto88
garwa4d
garwa4d
garwa4d
triadtoto
triadtoto
triadtoto
triadtogel
triadtogel
triadtogel
triad4d
triad4d
triad4d
triad4d
triad4d
triad4d
triadhk
triadhk
triadhk
triadhk
triadhk
triadhk
triadmacau
triadmacau
triadjitu
triadjitu
triadjitu
scatter99
scatter99
scatter99
scatter99
scatter99
sibayak99
sibayak99
sibayak99
sibayak99
sibayak99
sibayak99
sibayak99
sibayak99
boom138
emas69
emas69
rokettoto
rokettoto
rokettoto
rokettoto
bukitdita
kirintoto
kirintoto
triadsgp
triadsgp
triadsyd
triadsyd
torpedo99
torpedo99
torpedo99
torpedo99
premium138
premium138
premium138
premium138
premium138
premium138
bosslot138
bosslot138
bosslot
bosslot138
bosslot138
pusat69
pusat69
dompet69
dompet69
dompet69
dompet138
dompet188
dompet168
dompet123
harta69
triadslot
triadslot
triad303
138vip
138vip
triadtogel
triadtoto
triad4d
triadhk
triadhk
triad4d
triadtogel
triadjitu
triadmacau
boom138
garwa4d
scatter99
emas69
torpedo4d
nagatoto88
vinaslot
vinaslot
vinaslot
pwktoto

A Rare Unreported Case of Comminuted Bicondylar Hoffa’s Fracture
Volume 7 | Issue 3 | September-December 2021 | Page: 23-25 | Gaurav Gupta, Qaisur Rabbi, Maulin Shah, Vikas Bohra
DOI-10.13107/ijpo.2021.v07i03.118
Authors: Gaurav Gupta MS Ortho. [1], Qaisur Rabbi D Ortho. [1], Maulin Shah MS Ortho. [1], Vikas Bohra DNB Ortho. [1]
[1] Department of Orthopaedic, OrthoKids Clinic, Ahmedabad, Gujarat, India.
Address of Correspondence
Dr Maulin Shah
Consultant Paediatric Orthopaedic Surgeon, OrthoKids Clinic, Ahmedabad, Gujarat, India.
E-mail: maulinmshah@gmail.com
Abstract
A coronal plane fracture of the distal femur (Hoffa’s fracture) is very uncommon and usually occurs as a consequence of high velocity trauma. Bicondylar involvement of coronal femoral fractures is even less common, especially in children. To our knowledge, this is the first case report of a comminuted bicondylar Hoffa’s fracture in the paediatric age group managed by low profile solid locking screws.
A fourteen-year-old boy was referred with complaints of pain, swelling and deformity of the left knee after a fall from a height of approximately 10 feet. Clinical examination of the left knee revealed swelling and effusion with a low-lying patella and multiple superficial abrasions. X-ray of the left knee revealed bicondylar Hoffa’s fracture (Letenneur type III, Salter Harris type III). Computed tomography (CT) revealed a comminuted non-conjoint bicondylar Hoffa’s fracture with a low-lying patella. The fracture was approached through an anterior midline incision. Extensor mechanism of the knee was found intact. Fracture fragments were reduced anatomically and held in compression with long ball-tipped clamps. Four screws were placed in an antero-posterior (two screws for each condyle) and two screws in a medio-lateral direction to achieve a strong fixation construct. The screws were kept entirely in the epiphysis. At 12 months follow-up, the patient was walking with a normal gait, and full extension and 90 degrees of flexion at the knee. Quadricepsplasty was performed at 1 year to improve knee flexion. At final follow up of 2 years, he had full range of knee motion with no functional limitation.
Keywords: Hoffa’s, Bicondylar, Adolescent, Comminuted, Quardricepsplasty
References
1. White, E. A., Matcuk, G. R., Schein, A., Skalski, M., Maracek, G. S., Forrester, D.M., & Patel, D. B. (2014). Coronal plane fracture of the femoral condyles: anatomy, injury patterns, and approach to management of the Hoffa’s fragment. Skeletal Radiology, 44(1), 37–43.
2. Harna B, Goel A, Singh P, Sabat D. Pediatric conjoint Hoffa’s fracture: An uncommon injury and review of literature. J Clin Orthop Trauma. 2017;8(4):353–354.
3. Lal H, Bansal P, Khare R, Mittal D. Conjoint bicondylar Hoffa’s fracture in a child: a rare variant treated by minimally invasive approach. J Orthop Traumatol. 2011;12(2):111–114.
4. Hoffa’s A. Lehrbuch der Frakturen und Luxationen. Stuttgart: Verlag von Ferdinand Enke. 1904; p. 451.
5. Ul Haq R, Modi P, Dhammi I, Jain AK, Mishra P. Conjoint bicondylar Hoffa’s fracture in an adult. Indian J Orthop. 2013;47(3):302–306.
6. Giotikas D1, Nabergoj M1, Krkovic M1. Surgical management of complex intra-articular distal femoral and bicondylar Hoffa’s fracture. Ann R Coll Surg Engl. 2016 Nov;98(8): e168-e170.
7. Kondreddi V, Yalamanchili RK, Ravi Kiran K. Bicondylar Hoffa’s fracture with patellar dislocation – a rare case. J Clin Orthop Trauma. 2014;5(1):38–41.
8. Mak W, Hunter J, Escobedo E. Hoffa’s Fracture of the Femoral Condyle. Radiology Case Reports [Online]. 2008; 3:231.
9. Xiao, K., Chen, C., Yang, J., Yang, D., & Liu, J. An attempt to treat Hoffa’s fractures under arthroscopy: A case report. Chinese Journal of Traumatology. 2018 Oct; 21(5): 308–310.
10. Thompson TC. Quadricepsplasty to improve knee function. J Bone Joint Surg Am. 1944;26:366–79.
(Article Text HTML) (Full Text PDF)
Late Presentation and Reconstruction of Fingertip Crush Injury in a Child: A Unique Case Report
Volume 7 | Issue 3 | September-December 2021 | Page: 38-41 | Parag Lad, Sanket Tanpure
DOI-10.13107/ijpo.2021.v07i03.122
Authors: Parag Lad D Ortho. [1], Sanket Tanpure DNB Ortho. [1]
[1] Department of Orthopaedic, Jupiter Lifeline Hospital, Thane, Maharashtra, India.
Address of Correspondence
Dr. Sanket Tanpure,
Department of Orthopaedic, Jupiter Lifeline Hospital, Thane, Maharashtra, India.
E-mail: sankettanpure55@gmail.com
Abstract
Introduction: The fingertip is the most commonly injured part of the hand; therefore, fingertip injuries are among the most frequent injuries that surgeons are required to treat. Crush injuries of the fingertip are typically due to compression by a closing door. We report a late presentation of fingertip crush injury and its management on the dominant little finger in a child.
Case presentation: A 2-year-old male presented with infected and early necrosis of dominant hand little fingertip, caused due to door crush injury. The patient presented at 35 days with an exposed distal phalanx, marginal necrosis and partially healed, ulnarly-placed pulp of the fingertip. The parents of the child were counselled for one attempt of thorough debridement and consideration of pulp adipo-fascial flap repositioning to cover the distal phalanx. Local debridement and trimming of the pulp skin edges were carried out. The ulnarly displaced pulp was repositioned on the tip to cover the distal phalanx and sutured to the radial aspect of the nail fold with absorbable sutures. At 2 years follow up, the injured little finger was normal in cosmesis, function and nail growth.
Conclusion: Healing potential in children is good. Thorough debridement, nailbed and pulp reconstruction to cover the tip of distal phalanx and immobilisation for two weeks help to provide better cosmesis in the form of normal contour of the fingertip and movements, even in late presenting cases.
Keywords: Childhood crush injury, Fingertip, Late presentation, Debridement
References
1. Glicenstein J. and Haddad R. Management of fingertip injury in the child. In: Foucher G. (ed.), Fingertip and Nailbed Injuries. Churchill Livingstone, 1991: pp. 120-128.
2. Doraiswamy NV, Baig H. Isolated Finger injuries in chil¬dren-incidence and aetiology. Injury. 2000;31(8):571-3.
3. Fetter-Zarzeka A, Joseph MM. Hand and fingertip injuries in children. Pediatr Emerg Care. 2002;18(5):341-5.
4. Ljungberg E, Rosberg HE, Dahlin LB. Hand injuries in young children. J Hand Surg Br. 2003;28(4):376-80.
5. Fetter-Zarzeka A, Joseph MM. Hand and fingertip injuries in children. Pediatr Emerg Care. 2002;18(5):341 345.
6. Patel L. Management of simple nail bed lacerations and subungual hematomas in the emergency department. Pediatr Emerg Care. 2014;30(10):742-745.
7. Van Beek AL, Kassan MA, Adson MH, Dale V. Management of acute fingernail injuries. Hand clinics. 1990 Feb 1;6(1):23-35.
8. Kubus M, Andrzejewska E, Kuzanski W. Fingertip injuries in children treated in Department of Pediatric Surgery and Oncology in the years 2008-2010 [abstract only]. Ortop Traumatol Rehabil. 2011;13(6):547-554.
9. Innis PC. Office evaluation and treatment of finger and hand injuries in children. Curr Opin Pediatr. 1995;7(1):83-87.
10. de Alwis W. Fingertip injuries. Emerg Med Australas. 2006;18(3):229-237.
11. Macgregor DM, Hiscrox JA. Fingertip trauma in children from doors. Scot Med J. 1999;44(4):114-115.
12. Yorlets RR, Busa K, Eberlin KR, Raisolsadat MA, Bae DS, Waters PM, Labow BI, Taghinia AH. Fingertip injuries in children: epidemiology, financial burden, and implications for prevention. Hand. 2017 Jul;12(4):3427.
13. Giddins GE, Hill RA. Late diagnosis and treatment of crush injuries of the fingertip in children. Injury. 1998 Jul 1;29(6):447-50.
14. Karakas AO, Yuce E. Evaluation of pediatric fingertip injuries using etiology, demographics and therapy. The Medical Bulletin of Sisli Etfal Hospital. 2020;54(3):306.
(Article Text HTML) (Full Text PDF)
September-December 2021
Click On The Image
September-December 2021
Editorial
Volume 7 | Issue 3 | September-December 2021 | Page: 01 | Jayant S. Sampat
DOI-10.13107/ijpo.2021.v07i03.113
Authors: Jayant S. Sampath FRCSEd (Tr & Orth) [1]
[1] Department of Orthopaedics, Rainbow Children’s Hospital, Bangalore, Karnataka, India.
Address of Correspondence
Dr. Jayanth S. Sampath,
Rainbow Children’s Hospital, Bangalore, Karnataka, India.
E-mail: editor.posi.ijpo@gmail.com
Dear friends and colleagues
This issue of IJPO features original articles and case reports on a wide variety of paediatric orthopaedic conditions ranging from congenital deformities to infection and trauma. The POSI fraternity from India and around the globe have been sending in their submissions on a regular basis. This has enabled the IJPO team to publish twelve articles in this issue including 4 original papers, a new record for the POSI journal.
The “arm board” technique for the management of supracondylar fractures highlights the constant innovations being introduced into surgical practice by POSI members. Barick and colleagues have conducted a well-designed prospective study on walking age in children with clubfoot. Their work will help us to counsel parents of children with clubfoot appropriately. Other original articles on the management of osteoid osteoma and hemi-epiphyseodesis of the ankle add to the existing literature and provide new insights into the management of these conditions.
The case reports represent an eclectic mix of conditions from the rare “dysosteosclerosis” to the common problem of fingertip injuries in children. Each report is well written and presented to convey a clear message to the reader. On behalf of the Editorial Board, we commend each of the authors for their contribution and recognise the significant effort involved in seeing a submission through to publication. In the background, a large team of paediatric orthopaedic surgeons have provided their invaluable support for the peer-review process.
This issue also showcases the non-surgical skills of POSI members. Our cover page illustration is by Dr Easwar. T. R from Palakkad who dedicates his considerable artistic gift for charitable causes. Dr Taral Nagda has overseen the style and presentation of IJPO since its inception, in addition to creating previous cover page illustrations.
We have evolved substantially over the last 18 months. From reliance on invited article and symposia in the early days, IJPO is now composed entirely of original research work.
As always, we request interested POSI members to send in their submissions to the journal, volunteer to review articles and join the Editorial Board of the journal. Please visit our website www.ijpoonline.com for further details.
Jayanth S Sampath FRCSEd (Tr & Orth)
Editor, International Journal of Paediatric Orthopaedics (IJPO), POSI
editor.ijpo@gmail.com
(Article Text HTML) (Download PDF)
May-August 2021
Click on the page to view the entire issue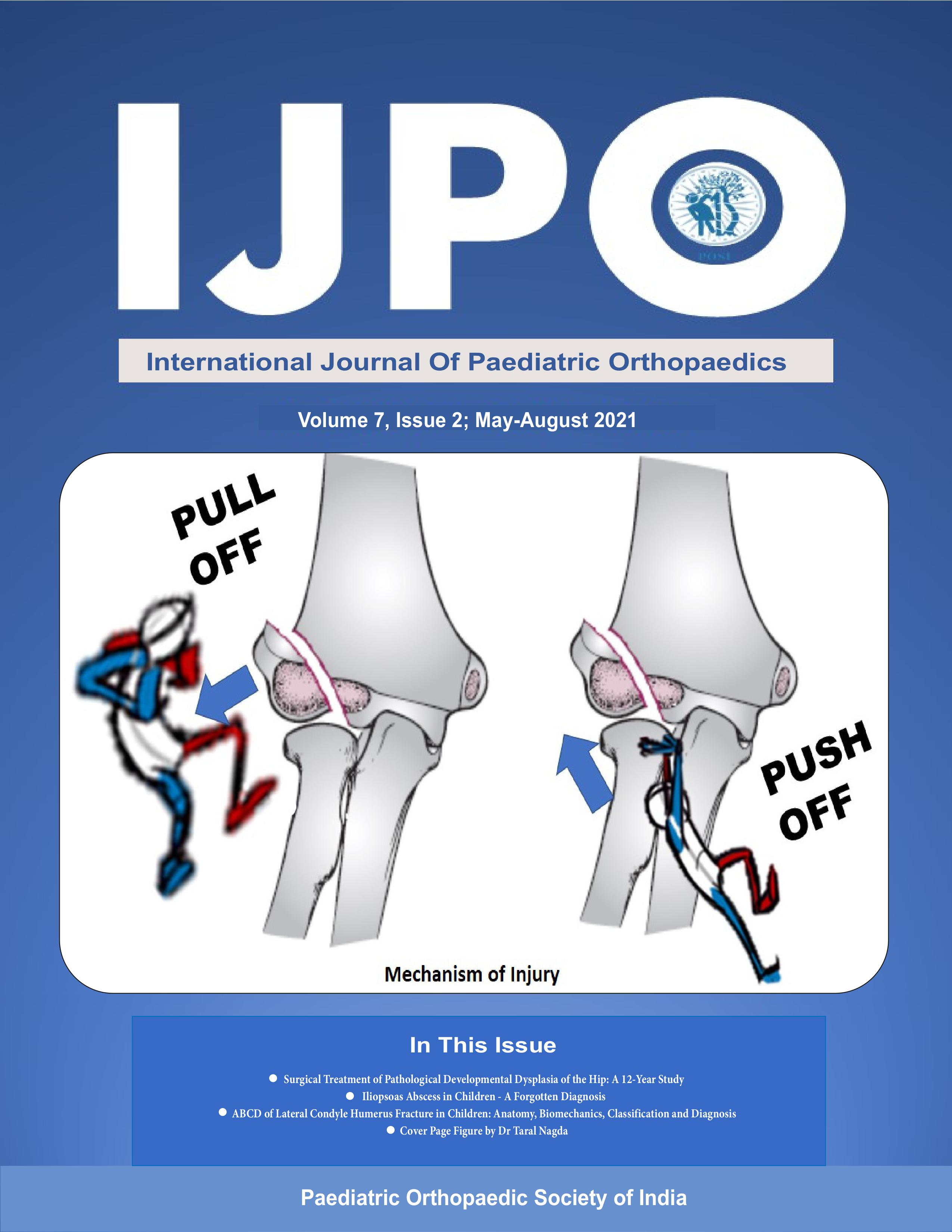
The Evaluation of Deformity Correction in Idiopathic Clubfoot During Ponseti Casting Sessions: Two Scoring Methods Depicted Graphically
Volume 7 | Issue 2 | May-August 2021 | Page: 12-16 | Anil Agarwal, Prateek Rastogi
Authors: Anil Agarwal [1], Prateek Rastogi[2]
[1] Department of Paediatric Orthopaedics, Chacha Nehru Bal Chikitsalaya, Geeta Colony, Delhi, India.
[2] Department of Orthopedics, Sharda Medical College, Greater Noida, Uttar Pradesh, India.
Address of Correspondence
Dr. Anil Agarwal
4/103, East End Apartments, Mayur Vihar Ph-1 Ext., Delhi-110096, India.
E-mail: rachna_anila@yahoo.co.in
Abstract
Background
We graphically analyzed the correction of total Pirani and Dimeglio scores and their subcomponents at sequential casting sessions for children with idiopathic clubfeet.
Methods
Correction of scores at weekly sessions was represented graphically. The tenotomy effect was accounted for separately. We classified 1st to 3rd casts as early, 4th and 5th cast midlevel, and beyond 5 as final casts to describe casting treatment.
Results
A total of 88 clubfeet (34 bilateral) in 54 patients were studied. Both total Pirani and Dimeglio graphs were characterized by a steep fall in early casts; subsequent minimal improvement in midlevel and final casts; later marked correction with tenotomy. Equinus in both scores stood as the most resistant deformity, showed full correction only following tenotomy. Dimeglio graphs captured coupling of various foot motions better over early casts than Pirani graphs.
Conclusions
Both Pirani and Dimeglio scores can adequately guide caregivers to progressive deformity correction in clubfoot.
Keywords: Clubfoot, CTEV, Pirani, Dimeglio, Scores, Graphs
References
1. Staheli L. Clubfoot: Ponseti management. Seattle, WA: Global HELP; 2009.
2. Pirani S, Naddumba E, Staheli L. Ponseti Clubfoot management: Teaching manual for healthcare providers in Uganda. Seattle, WA: Global HELP; 2008.
3. Chaudhry S, Chu A, Labar AS, Sala DA, van Bosse HJ, Lehman WB. Progression of idiopathic clubfoot correction using the Ponseti method. J Pediatr Orthop B. 2012;21: 73-78.
4. Lampasi M, Trisolino G, Abati CN, Bosco A, Marchesini Reggiani L, Racano C, et al. Evolution of clubfoot deformity and muscle abnormality in the Ponseti method: evaluation with the Dimeglio score. Int Orthop. 2016;40:2199-2205.
5. Lampasi M, Abati CN, Stilli S, Trisolino G. Use of the Pirani score in monitoring progression of correction and in guiding indications for tenotomy in the Ponseti method: are we coming to the same decisions? J Orthop Surg (Hong Kong). 2017;25:2309499017713916
6. Agarwal A, Shanker M. Temporal variation of scores along the course of the Ponseti treatment in older children: A ready guide to progress of treatment. J Pediatr Orthop. 2020;40:246-250.
7. Pirani S, Outerbridge HK, Sawatzki B, et al. A reliable method of clinically evaluating a virgin clubfoot evaluation. In: Proceedings of the 21st SICOT World Congress, Sydney, Australia, 18-23 April 1999.
8. Diméglio A, Bensahel H, Souchet P, Mazeau P, Bonnet F. Classification of clubfoot. J Pediatr Orthop B. 1995;4:129-136.
International Journal of Paediatric Orthopaedics | May-August 2021; 7(2): 12-16.
(Article Text HTML) (Download PDF)