History of Treatment, Classifications, Natural History and Prognosis with respect to Recurrence
Volume 2 | Issue 2 | May-Aug 2016 | Page 12-16|Binoti Sheth1, Bhaskaranand Kumar2
Authors :Binoti Sheth[1], Bhaskaranand Kumar[2]
[1]Lokmanya Tilak Medical College & Sion Hospital, Mumbai. India
[2] Hand Surgical Services, Kasturba Medical College & Hospital, Manipal – 576 119, Karnataka, India.
Address of Correspondence
Dr Binoti Sheth
Department of Orthopaedics, Lokmanya Tilak
Medical College & Sion Hospital, Mumbai. India
Email: binotisheth@yahoo.com
Abstract
Clinical presentation of radial club hand deformity varies from mild hypoplasia to complete absence of radius. Various classification systems are described for radial club hand deformity as the treatment is based on the severity of affection. Treatment of radial club hand has progressed over the years from no treatment to conservative treatment to aggressive surgical correction. Recurrence after the surgical treatment is one of the challenging problems in this anomaly. History of treatment, advances and modifications of treatment, natural history and recurrence with respect to treatment have been described here.
Key words: Radial club hand, classification, treatment, recurrence
Introduction
In 1733, Petit first described radial club hand in an autopsy of a neonate with bilateral club hands and absent radii. If untreated, the deformity does not appear to worsen over time, but there is limitation in prehension and the hand is used primarily to trap objects between it and the forearm. Lamb found that the activities of daily living are not significantly affected in unilateral involvement, but bilateral involvement reduces the activities by one third. In radial club hand, ulna length at birth is known to be approximately 50-75% of the normal ulna length. This limb length discrepancy normally persists throughout growth. According to the literature, the ulna may finally be shortened by as much as 40% of its normal length.[1] There is general agreement favouring surgical correction at 3-6 months of age in children with inadequate radial support of the carpus.
Classifications:
Various classification systems have been described for radial club hand deformity. Most useful and currently accepted classification is modification of that proposed by Heikel.[2] In this classification system, four types are described.
Type 1: (short distal radius)
In this type, the distal radius epiphysis is present but is delayed in appearance. The proximal radial epiphysis is normal. The overall length of the radius is slightly less ,but the ulna is not bowed. (Fig.1)
Type 2 : (hypoplastic radius)In this type both proximal and distal radial epiphysis are present, but are delayed in appearance. Due to this there is moderate shortening of the radius and thickening and bowing of the ulna.(Fig. 2)
Type 3:(Partial absence of radius) Here , there is partial absence of proximal, middle or distal third of radius, distal being most common. Ulna is thickened and bowed. The carpus is usually radially deviated and unsupported. (Fig. 3)
Type 4 : (total absence of radius)
This is the most common type of radial club hand. Here ,there is radial deviation of the carpus, palmar and proximal subluxation, frequent pseudoarticulation with the radial border of distal ulna.There is shortening and bowing of the ulna. (Fig. 4)
Bayne and Klug [3] have described a radiological classification system with four types.
Type 1: Deficient distal radial epiphysis
Type 2 : Deficient distal and proximal radial epiphysis.
Type 3 :Partial aplasia of radius(present proximally)
Type 4 :Total aplasia of radius(complete absence)
Type 4 is the most common type of radial club hand.
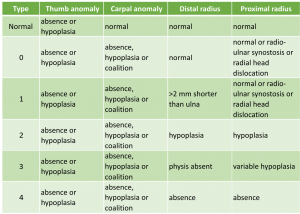
A fifth type was added by Goldfarb et al [4] describing a radial dysplasia with participation of the humerus. James and colleagues expanded the classification by including deficiency of the carpal bones with a normal distal radius length as type 0 and isolated thumb anomalies as type N.
Variable degrees of thumb deficiencies are frequent with all patterns of radial club hand.(Fig. 5) Manske et al.[5] have devised a global classification system of radial longitudinal deficiency.(Table 1) They have included thumb and carpal abnormalities also in the classification. Carpal anomaly implies hypoplasia, coalition, absence or bipartite carpal bones .Hypoplasia and absence are more common on radial side of carpus and coalitions are more common on ulnar side. X rays must be taken beyond 8 years to allow for ossification of carpal bones.
History of Treatment:
The goal of treatment in radial club hand is to correct the wrist deformity, to maintain the corrected position, to provide wrist-like mobility, to preserve longitudinal growth capacity of ulna and to achieve an acceptable cosmetic result.
Non Surgical Treatment
Riordan [6] recommends applying a long arm cast as soon after birth as possible. The cast is applied in three stages using a technique similar to that used in clubfoot casting. The hand and wrist are corrected first and then the elbow is corrected as much as possible. The correction may be achieved in the infant but according to Milford, casting and splinting is often impractical in a child of age less than 3 months. Lamb [7] reported that elbow extension contracture can be improved by splinting with hand and wrist in neutral position. Current recommendation of treatment is to start from birth with stretching and splinting in order to lengthen the soft tissues and facilitate the reduction of the deformity. A large retrospective review of 446 patients including 137 patients managed non surgically and 309 patients managed with either a centralization or radialization procedure, found that those managed surgically had improvement in appearance and function, including improved alignment, range of motion and strength [8].
Surgical Treatment
Initial surgical treatment described by Bardenheuer was ulnar osteotomy to correct bowing and splitting of distal ulnar for insertion of carpus. Hoffa in 1890 performed a distal transverse osteotomy of ulna to simply realign the ulna. Albee [9] in 1919 attempted to create a radius with a free tibial graft. These surgeries did not give satisfactory result.
Centralization:
In 1894, Sayre [10] described the centralization technique that has now become the treatment of choice across the world. Sayre had described shaping of the distal ulna and notching of the carpus.
Although maintaining alignment, this procedure resulted in a high incidence of spontaneous ulnocarpal fusion with inherent loss of motion and reduced growth potential of the ulna. Many authors have subsequently modified this procedure in an attempt to decrease the potential morbidity while maintaining wrist position. Lidge [11] in 1969 introduced an improved method where ulnar epiphysis was preserved at the expense of central carpal bones that had to be resected. Although early results were good, late results were less satisfactory. Lamb recommended creation of carpal notch to stabilize the carpus on the ulna. He suggested depth of the notch to be equal to the transverse diameter of the distal ulna and this required removal of all of the lunate and most of the capitate. As against this, Watson et al.[12] suggested not to excise any of the carpus because of the possibility of affecting growth of the forearm. Buck-Gramcko (1985) and Bayne and Klug also suggested not to remove any of the carpus.
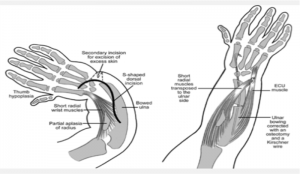
Different incisions and surgical approaches for centralization procedure have been described due to the problems of significant skin tension on radial side following ulna repositioning. Manske and McCarroll [13] preferred transverse ulnar incision, as described by Riordan, removing an ellipse of skin (Fig. 6)
Watson, Beebe and Cruz [12] preferred ulnar and radial z-plasty incisions to allow removal of the distal radial anlage which they believe is essential. Lamb (1972) [14] and Buck Gramcko (1985) described S-Shaped incision for better exposure. (Fig. 7)
Evans described dorsal bilobed skin flap to provide additional skin on radial side and take up excess on the ulna side of the wrist. This gives good access to wrist joint and surrounding soft tissue structures.(Fig. 8 )
DeLorme (1969) [15] first suggested intramedullary fixation of carpus on the ulna. Most authors now prefer to use K wire to secure alignment of long or index metacarpal with the ulna for at least 6 weeks. Still the recurrence rates are high. To overcome the recurrence tendency, additional procedures were introduced including collateral ligament reconstruction, soft tissue balancing by tendon transfer and leaving K wire for as long as possible (preferably several years) Bora et al [16]. recommended adjunctive tendon transfer. FDS from central digits was transferred around the postaxial side of the forearm into the dorsal aspect of metacarpal shaft. Hypothenar muscles were transferred proximally along ulnar shaft. ECU was transferred distally along the shaft of the metacarpal of little finger. However, this procedure failed to prevent 25-35 degrees of recurrent radial deviation. Bayne and Klug recommended transfer of FCU into the distally advanced ECU to help prevent radiovolar deformity.
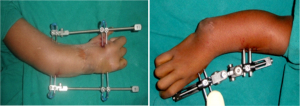
Pre-centralization distraction:
Another recommendation to prevent recurrence was to use soft-tissue distraction before centralization (Fig. 9). Kessler [17](1989) described a technique to passively distract the soft tissue with an external fixation before centralization. Goldfarb et al reported on soft tissue distraction precentralization and noted that the centralization could be performed effectively and without tension after distraction, which averaged 6mm. Nanchahal and Tonkin [18] reported a similar experience, noting that carpal realignment was possible in 5 of 6 patients who underwent preoperative distraction, but only in 1 of 6 patients treated without distraction. Kanojia et al [19] reported similar experience with an external fixator and noted that early application can lead to completion of surgical treatment by 10 months of age in the vast majority of patients. Sabharwal et al[20] used Ilizarov for soft tissue distraction prior to centralization, considering it to be more comprehensive achieving physiologically sound distraction. Ilizarov has certain advantages over external fixator, as there is option of placing multiple bony anchors in different planes, application of translational hinges corresponding to the apex of the deformity. Bhat et al.[21] used MAC system (Multi axial correction) for correction of triplanar angulation, translation, rotation and limb length discrepancy. They found it useful especially in adolescent age group with previous failed soft tissue procedures. Dana et al.as well as Prokopovitch [22] and Kessler have reported small series of radial club hand deformities treated by external fixator application to gradually stretch the soft tissues to facilitate centralization.
Radialization:
Even with soft tissue distraction prior to centralization, there is high incidence of unsatisfactory results. Buck-Gramcko in 1985 developed a modified technique to improve the outcome. It is called ‘radialization’ [23]. In this technique, the hand is brought with its radial carpal bones over the head of the ulna and fixed with a K wire in moderate ulnar deviation to produce some overcorrection(Fig.10). Also ECR and FCR muscles are transposed to weaken the forces for radial deviation, thereby preventing recurrence while a better muscle balance is established. Both modifications tend to improve mechanical conditions which are prerequisites to maintain hand and forearm in proper relation. Also, in this technique, the resection of carpal bones can be avoided to help increase total arm length and improve range of motion. Buck Gramcko used this technique in 30 cases and found satisfactory results. With improved function and further growth, the distal end of the ulna became broad like a radius.
Ulnar lengthening:
Ulnar lengthening was another technique used to increase forearm length, typically with the aid of a circular frame such that correction of the radial deviation can occur simultaneously. Farr et al [24] recommended lengthening procedure to be performed in school age children (8-10 years) to gain sufficient limb length for performance of ADL including perineal care in adolescence and adulthood. A second lengthening step may follow after growth cessation, depending on the functional outcome of the first procedure. They reported on 8 cases in 6 patients and noted that initial post surgical gains were not maintained and there was recurrence of radial deviation at an average 4 years follow up. Two major complications occurred, including an ulnar fracture after frame removal and insufficient regenerate during lengthening. Peterson et al [25] described 9 children who underwent 13 lengthenings after previous centralization procedures. The average gain in length was 4.4 cm (range 1.8-8.0 cm). All patients had at least one pin site infection that was treated with antibiotics. 4 patients required additional procedures including internal fixation and bone grafting for delayed union in 3 patients and wrist arthrodesis for recurrence in 1 patient. Yoshida et al[26] investigated the growth of the ulna after repeated lengthenings. After the initial lengthening, the average length improved from 57% to 89% of the normal side, but then regressed to 70% whereas after the second lengthening, the average length was 102% but regressed to 83%. Bone growth was markedly decreased after the second lengthening. Hence, when multiple lengthenings are performed the second one should be done after skeletal maturity (Fig. 11). Sestero et al [27] assessed the ulnar length and growth of 72 limbs treated either surgically or non surgically over 80 years. They found that non surgically treated extremities attained 64% of normal length, whereas patients who underwent surgery achieved 48% (notched centralization) to 58% (non notched centralization) of normal ulnar length. They also calculated an average annual ulnar growth of 2.6 cm after surgery, compared with 3.6 cm for patients treated non surgically. However, a recent study of 446 affected hands reported that surgical treatment was superior to conservative treatment in terms of appearance and function. Hill et al.[28] have suggested that full restoration of length is not necessary for this procedure to have a successful outcome. Recurrence of deformity after forearm lengthening has not been well described. Kawabata et al.[29] observed a tendency towards recurrence of ulna bowing and radial deviation in 4 of 7 patients, showing a final angular deformity of 19 degrees.
Radial lengthening:
Matsuno et al [30] described 4 cases of mild (Bayne and Klug type I and II) radial club hand treated with radial lengthening and simultaneous soft tissue distraction between ulna and 3rd metacarpal. Three of the four patients required several lengthenings to correct the recurring discrepancy between the radius and ulna. Only two of the four patients had acceptable function and appearance after the multiple procedures. In one patient, lengthening was abandoned owing to severe bone absorption at the distal end of the radius.
Vascularised metastarsophalangeal transfer:
In 1920, an attempt was made to reconstruct the radius with bone graft to support the carpus. In 1945, non vascular epiphyseal transfer was attempted for treatment of radial club hand, but the results were disappointing, with disrupted ulnar growth plate and increase in limb length discrepancy. Also, there was inadvertent ankylosis / arthrodesis of wrist and loss of radial support. Vikki [30] reported the results of vascularised second metatarsophalangeal joint on 24 limbs with an average follow up of 11 years. The average radial deviation at final follow up was 280, the average active wrist total arc of motion was 830 and the average length of the ulna was 67% of the contralateral side. But complications were present in more than 50% of patients, including failure of the transfer and subluxation of the joint.
Post-operative assessment:
The outcome of various surgical procedures can be assessed by cosmetic appearance, total wrist arc of motion and certain radiological measurements as described by Manske et al.[13] HFA (Hand-FA angle) is the intersection angle between long axis of the long metacarpal and distal ulna, as measured on AP x-ray. Minus’ HFA refers to the hand and long axis of long finger metacarpal distal axis directed in ulnar deviation with respect to distal ulna. This is the more desired position. HFP (Hand FA position) refers to the distance in mm between base of little finger metacarpal and distal ulna. If proximal pole of little finger metacarpal was ulnar to the axis of distal ulna, the position (HFP) recorded as positive mm, a change in ulnar direction was considered an improvement in the position of hand. Ulnar bowing was defined as the angle between the intersection of the proximal and distal ulnar bi sector lines. The goal of treatment in radial club hand is to achieve slight overcorrection with ulnar deviation of hand and ulnar translation of hand and wrist at the end of treatment.(Fig. 12)
Recurrence:
Despite various advances in the surgical treatment of radial club hand, recurrence of radial angulation and ulna bowing is common. A possible cause may be the soft tissue, which remains pathologic after centralization or radialization. After consecutive lengthening and relative realignment of the forearm, the altered fibrous muscles and connective tissue lead to progressive rebowing of the ulna and a radial shift of the wrist. Precentralization distraction aids in soft tissue balancing at the time of centralization, but it is unknown whether the technique will improve maintenance of alignment with longer follow-up. Deformities noted to be more severe preoperatively were more likely to recur. Also, recurrence was associated with young age (less than 12 months) at index procedure and immediate post operative radial deviation position. It is advisable to inform the parents (and patients) at the time of centralization, that the deformity may recur. Lamb reported 3 recurrences of volar angulation after 31 centralization procedures [14]. Damore et al[32] reported that the mean total angulation (radial deviation and ulnar bow) improved from 830 before centralization to 380 after, but recurred to 630 radial deviation at a mean 6.5 years after centralization. Geck et al [34] performed survivorship analysis of 29 radial club hand treated with centralization or radialization, with an end point of revision surgery for recurrence. At 5 years, one third of patients presented with a recurrent deformity that was subsequently treated by revision. According to Pike et al.[33] post centralization recurrence of radial angulation to greater than 450, an inability to actively extend the wrist to within 250 of neutral (i.e. 250 of flexion) or both, are considered as indications for re-surgery. Treatment of recurrent deformity after centralization is problematic; repeated centralization is likely to fail again because of the instability of the hand and carpus at the end of a single forearm bone. The preferred treatment after a failed centralization procedure is ulnocarpal arthrodesis in skeletally mature or an epiphyseal arthrodesis when the distal ulna physis is still open. Epiphyseal arthrodesis showed no disturbance in extremity growth when performed in skeletally immature extremities when the surgical principles for preserving the epiphysis were carefully followed. There is always a concern about the irreversible feature of a wrist fusion in a young patient. To address this concern, a temporary arthrodesis is offered to patients to allow the patient to make an informed decision, the wrist is stabilized in surgery with percutaneous K wires holding the ulno-carpal joint in the anticipated position of fusion. If the patient likes the position, epiphyseal arthrodesis is performed in 1 to 2 weeks, if the patient does not like the position, K wires are removed and the wrist returns to its former position.
There are several treatment options for radial club hand, including non surgical management; centralization, radialization or ulnarization; ulnocarpal arthrodesis; soft tissue procedures including distraction; ulnar lengthening; and vascularized second metatarsophalangeal joint transfer. The most common procedure performed currently is soft tissue distraction followed by a wrist realignment procedure such as centralization, or radialization. Ultimately, a procedure is needed that can correct and maintain the deformity, yet permit growth with a low complication rate.
References
1. Louri GM,Linse RE: Radial longitudinal deficiency:A review and update Hand Clin. 1998;14(1):85-99.
2.Heikel H.A.:Aplasia and hypoplasia of the radius Acta Orthop Scand Suppl 39:1,1959
3. Bayne LG, Klug MS. Long-term review of the surgical treatment of radial deficiencies. J Hand Surg Am. 1987 Mar;12(2):169-79.
4. Goldfarb CA, Manske PR, Busa R, Mills J, Carter P, Ezaki M. Upper-extremity phocomelia reexamined: a longitudinal dysplasia. J Bone Joint Surg Am. 2005 Dec;87(12):2639-48.
5.James MA, McCarroll HR Jr, Manske PR: The spectrum of radial longitudinal deficiency: a modified classification J Hand Surg Am. 1999 Nov.24(6):1145-55
6. Riordan DC. Congenital absence of the radius. J Bone Joint Surg Am. 1955
Dec;37-A(6):1129-39
7.Lamb DW. Radial club hand. A continuing study of sixty-eight patients with one hundred and seventeen club hands. J Bone Joint Surg Am. 1977 Jan;59(1):1-13..
8. Kotwal PP, Varshney MK, Soral A. Comparison of surgical treatment and nonoperative management for radial longitudinal deficiency. J Hand Surg Eur Vol. 2012 Feb;37(2):161-9.
9.Albee FH:Formation of radius congenitally absent:condition seven years after implantation of bone graft, Ann. Surg.87:105,1928
10.Sayre RH. A contribution to the study of club hand, Trans Am Ortho Assoc 6:208, 1893
11. Lidge RT. Congenital radial deficient club hand, J Bone Joint Surg 51-A 1041, 1969
12. Watson HK, Beebe RD, Cruz NI. A centralization procedure for radial clubhand. J Hand Surg Am. 1984 Jul;9(4):541-7.
13.Manske PR, McCarroll HR Jr, Swanson K. Centralization of the radial club hand: an ulnar surgical approach. J Hand Surg Am. 1981 Sep;6(5):423-33
14. Lamb DW. The treatment of radial club hand. Absent radius, aplasia of the radius, hypoplasia of the radius, radial paraxial hemimelia. Hand. 1972 Feb;4(1):22-30.
15.DeLorme TL:Treatment of congenital absence of radius by transepiphyseal fixation J Bone Joint Surg 51-A:117,1969
16.Bora FW, Osterman AL, Kaneda RR:Radial club hand deformity:long term follow up J Bone Joint Surg 63-A: 741,1987
17.Kessler I:Centralization of the radial club hand by gradual distraction, J Hand Surg 14-B:37,1989
18. Nanchahal J. and Tonkin M.A. : Pre-operative distraction lengthening for radial longitudinal deficiency J. Hand Surg. Br. 1996:21:pp 103-10.
19. Kanojia R.K., Sharma N, and Kapoor S.K.: Preliminary soft tissue distraction using external fixator in radial club hand. J. Hand Surg, Eur. Vol. 2008; 33:pp 622-627.
20.Sabharwal S et al.: Pre-centralization soft tissue distraction for Bayne type 4 congenital radial deficiency in children J Paed Orth 2005, 25(3):377-81
21.Suneel Bhat et al.MAC system in the treatment of radial club hand J Child Ortho 2009 Dec 3(6):493
22.Prokopovich VS; Aligning of the length of the forearm bones in the congenital club hand in children Orthop Traumatol Protez 1:51,1980
23.Buck –Gramcko D: Radialization as a new treatment for radial club hand J Hand Surg 10-A(pt 2):964,1985
24.Farr S, Petje G, Sadoghi P: Radiographic early to mid term results of distraction osteogenesis in radial longitudinal deficiency J Hand Surg Am 2012: 37,2313-2319
25.Peterson BM, McCarroll HR,James MA:Distraction lengthening of the ulna in children with radial longitudinal deficiency J Hand Surg Am 2007,32:1402-07
26.Yoshida K,Kawabata H,Wada M:Growth of the ulna after repeated bone lengthening in radial longitudinal deficiency J Paed Ortho 2011 :31, 674-678
27.Sestero AM, Van Heest A,Agel J:Ulnar growth patterns in radial longitudinal deficiency J Hand Surg Am 2006 Jul- Aug,31(6):900-7
28. Hill RA, Ibrahim T, Mann HA, Siapkara A. Forearm lengthening by distraction
osteogenesis in children: a report of 22 cases. J Bone Joint Surg Br. 2011 Nov;93(11):1550-5.
29.Kawabata H, Shibata , Masotami T, Yasui N:Residual deformity in congenital radial club hands after previos centralization of the wrist, ulnar lengthening and correction by the Ilizarov method J Bone Joint Surg Br 1998 Sept 80(5):762-5
30.Matsuno T, Ishida O,Sunagawa T, Suzuki O:Radius lengthening for the treatment of Bayne and Klug type 2 and 3 radial longitudinal deficiency J Hand Surg Am 2006:31, 822-829
31. Vikki SK: Vascularised metatarsophalangeal joint transfer for radial hypoplasia Semin Plast Surg 2008:22, 195-212
32. Damore E; Kozin S.H. Thoder J.J. and Porter S : The recurrence of deformity after surgical centralization for radial clubhand J. Hand Surg. Am-2000; 25:pp 745-751.
33. Pike J.M., Manske P.R., Steffen J.A. and Goldfarb C.A. :Ulnocarpal epiphyseal arthrodesis for recurrent deformity after centralization for radial longitudinal deficiency J. Hand Surg. Am. 2010; 35:pp. 1755-61.
34. Geck MJ, Dorey F, Lawrence JF, Johnson MK. Congenital radius deficiency:
radiographic outcome and survivorship analysis. J Hand Surg Am. 1999 Nov;24(6):1132-44.
| How to Cite this Article: Sheth B, Kumar B. History of Treatment, Classifications, Natural History and Prognosis with Respect to Recurrence. International Journal of Paediatric Orthopaedics May-Aug 2016;2(2):12-16. |