License
International Journal of Paediatric Orthopaedics is licensed under a
https://creativecommons.org/licenses/by-nc-sa/4.0/
Publisher
Official Journal of:
Paediatric Orthopaedic Society of India (POSI)
Publisher:
ResearchOne Publishing House,
An "Indian Orthopaedic Research Group (IORG) initiative.
IORG House,
A-203, Manthan Apts, Shreesh CHS, Hajuri Road,
Thane [West], Maharashtra, India.
Pin Code- 400604
Tel- 02225834545
Publisher Email: indian.ortho@gmail.com
Editor Email: editor.ijpo@gmail.com
pwktoto
holyslot123
Amanah99
Rupiah777
horastogel
cuanslot
okta138
tango168
lotus777
bostoto138
medali69
milojitu
Lotre78
lux77
Gorilatoto
Hoki338
Dewapoker77
baikbet
sule78
lavatoto
uang138
Merak99
porto4d
hemattoto
Kaca138
puri138
anginbet
Joglo4d
juragantogel
Mahyong69
sojubet
sakti777
StarJoker69
grab78
spacetogel
jarum169
Kudatoto
pangkalanbet
ten88
opera99
satelit69
koin88
pondok338
jaring338
pubtogel
milo338
thor388
deltatoto
bdjitu
mirana99
amat123
autobet123
Shio77
gemoy188
planet888
Maria99
makmurwin
pakdejp
geber777
lato777
Melatibet
bankslot
hujantogel
coco69
Rusa69
Apollo303
sule777
namabet
Mars77
moon138
Pancingslot
Pulaubet
rumah88
cumi303
prada68
versace138
Koala4d
lobby69
lux78
usaha4d
kambingtogel
Musangtoto
delta777
Jeweltoto
pos188
lava77
maluku303
kompor88
luckslot
Lotre169
lotus68
raffi169
tambang388
ratuzeusqq
dinasti99
Modalhoki108
asiajitu
judi78
astra78
partaiqq
rumah69
Meriam123
evosbet88
Sayangbet
Lilin4d
Cemaraslot
furla69
kumis4d
Bandungslot
japan78
hokislot123
hulk303
Pragmatic69
chivas69
krisna188
Lyonslot
ASIABET168
topislot
bola123
ultra365
ios55
kompor77
sinaga138
kelapabet
padang777
Rajawin777
Jakarta88slot
Becak168
babetogel
primaslot
Moonslot
palu338
pulautogel
botaktogel
platinum138
cici169
gunturtogel
Kacang4d
dewabet138
spin388
homebet69
bursatoto
mami4d
pasbet
aduhoki
lava69
pagoda388
meledak99
dalang138
Gama188
dino777
papua338
darat123
hokiwin55
Cobra777
Merak88
crown78
preman77
grab188
terminal388
apiwin
madura78
sinar303
Dupawin
Santuy188
kera388
Modalhoki68
omuslot
Peri123
divabet
macau388
Angsa138
keris69
DOMINOPKV
Bos69
Sawitjitu
jaring99
layar77
tayototo
taro168
pejuang388
next88
harapan168
hemat123
Shio88
apidewa77
parisjp
pohon69
Lotre777
taruna123
asean168
giga69
StarJoker123
tempat99
Sisir4d
Tokek78
bosstogel
pakdeslot88
wisslot
rumah108
dominoslot
cola123
jili88
kompas77
bisnis77
kungfu69
Arjuna77
sensa123
Piramida4d
gacor365
pucuk777
Lotre123
wayang777
Gama178
WLA88
langitmpo
Robot4d
kumbang123
Logam4d
Sawit138
Bca168
petir88
tokyobet
tempo123
Permen178
Gacorbos99
wiratogel
LUNAS805
sateslot
barbar188
maxwin123
pecahtogel
Menang77
demotogel
trisula4d
candy138
bostoto188
demo388
citatogel
SIRKUIT138
Boy4d
Kalaslot
formulabet
Kode99
icon55
domino123
cartel303
jingga4d
Luxuryqq
space168
Legenda4d
porto169
api69
ASIAMPO77
wiki69
fasslot
cincin77
rajatoto68
Merak78
batastogel
gem108
buku99
furlabet
versace168
Sayang777
marvel365
kumis138
sushitoto
cbototo
latar77
Hadiah4d
solusi138
udara4d
sayang188
maha777
milo55
taro303
Dunia88
sejuta188
Dewapokertogel
Luxurygg
KOBOYPOKER
Aksara77
amat303
unggul123
oris77
kingdomjitu
merci4d
Aontoto
gemoyslot
geloratoto
layar69
winning138
sobet78
klik303
gilagg
bantamtoto
Sbo4d
Tombol4d
maya303
spin6d
sumo123
lambe88
barbar88
kadobet168
solid169
oasis365
karo303
duta69
sumo88
Pandawa123
ipar777
bengkelslot
macanslot
abc69
judolbetqq
Laku123
obor77
Lampion4d
memori77
jepang169
plntoto
ASIAPKV
Duyung88
Hijau123
dewanslot
MAXWIN888
SUARABET77
empirebet
Kucingtoto
kakek138
idr188
coca123
sisri77
jamu123
cumi99
fire123
persentogel
moon4d
dutabet
jaring365
Bigwin178
Gacorbos169
toto388
evosgamingg
kado99
WLA55
kadal303
rumah168
Poker138
Aztectoto
gasing78
extrabet
urban168
Topengslot
planet388
Angkatoto77
mulia88
qq69
luck388
epictogel
GACORBOS
icon169
atlas169
bentototo
jamu4d
libas169
holiday69
hulk77
skor77
karo168
colekbet
Bendera99
suhu4d
Dayak123
radentogel
KOBOY888
memori108
lajubet888
JUARAWIN88
BIMO77
jokerbetqq
AREASLOTO
juara77
dewi138
DEWIBET777
nusapoker
jilibet
Ikan303
kadalslot
depototo
harum123
pawang88
krisna123
madu55
Khusustogel
taktik388
Wahana4d
ovo168
mesinslot
Gogo90
bromo99
Badutjitu
Mega777
sentosa69
kamus168
Tigerslot
tempatslot
wazebet
sekai777
airtogel
Agen99
colek777
pasang388
pigi388
Angkatoto123
batam69
kudetabet69
mewah123
fuji338
papua78
murahpoker
cincin365
memori69
hantu78
anak777
Kapten99
Nanas188
Glory77
wiki78
PEDANGBET
mahjongs138
ipar78
motoslot88
POV99
bingo4d
ratuslot777
YUPI188
ASIASLOT888
fire777
pasti138
batam777
julietslot
iklan88
kamus77
sobet99
capital99
Sicbo4d
paris4d
daya365
amat168
roslot55
Kaktusslot
cakra123
Abu123
krisna77
guntur365
PEDANGJITU
panca123
Kodok123
ASIAKING777
JPSLOT168
wuling88
kaya77
KOBOIBOLA
garpu777
kingbet169
pir69
extra188
oren77
cair365
kingdomjp
dewaslot138
nagapoker777
cici138
Daun777
surga6d
holyslottoto
jakarta303
dinasti777
suara78
Mbah4d
HOKIOM88
zona77
unggul169
tempat123
Arus138
retro388
mampirtoto
sulaptogel
nagawin168
pecah188
bangsa338
ASIAHOKI88
neopoker
mesin188
canduslot777
dino78
asus88
Mangga4d
kumistogel
nama88
kkslot55
LUNA999
Tokcer69
Logam303
kkslot108
lgo188
gemoy777
ultra99
tahunslot
ligajp88
kampusslot
babe69
macau128
taktik123
kado338
Angsa77
latarslot
juliet777
lavaslot
suburbet
doyan77
ladang77
Dupaslot
YUPIBET
AREA188
betagg
usaha169
AREAWIN88
megawinbet
Tokcer168
mandiri99
MANTAP138
mahal99
Gobertogel
abc77
mulia99
bonus303
kembar388
sensatogel
atom188
gebyar77
baik388
balon138
Master77
ovo338
gaco169
edanbet
pistolslot
air169
kembang169
dna303
wigo123
ladangslot
pasang338
suryatogel
DOMINOBET77
kembar188
diva388
pohonjitu
Sakuraqq
kumis168
ASIATOTO777
Premium188
rupiah4d
CERIAPOKER
KAYA78
kebunbet
sawi69
pub365
pesiar69
Wild777
Tores777
paus168
bom108
Dollarjitu
vegas77
wis338
Kancil69
angkasaslot
Dolan138
semangat303
jaritogel
daun69
nova123
darat303
SERUBET88
selat123
hantu88
serbatoto
balon123
tenbet
padi78
benuawin
Sensa188
Emas88
Rajawalitogel
musangtogel
sarana78
sugar365
lexus108
bom123
kso123
luck4d
puncak88
vista123
muara69
Rutantoto
ceria88
RAFI777
alasbet
durentoto
mpomaster
cipitbet
usaha138
leobet
mantra168
Akun188
Nanastogel
alexa88
Tombol168
slotbom68
solid78
gunturslot
sake138
Gloryslot
luck77
raksasa138
mildbet
Doku123
Yakuza777
bostoto77
jutawan168
odin123
lampu168
cumi168
mega169
puri188
petatogel
dadu168
mahadewa168
karirtogel
istana88
serbu123
kumbang99
pulau169
Sarangslot88
muliaslot
tiktoktoto
retro4d
ayo68
Dugem88
jepe338
bns99
leo303
turbo77
timur77
baiktogel
masterbet123
Mansionslot
petirslot
retro69
unggul168
POV69
musik168
kapaljudi777
Habanero138
marvel188
kejubet
ios99
Ninjaslot
permen169
fix338
koi138
madura168
gerbang338
desa77
sushi168
Ikanslot
opera123
oren365
luckbet
Rusa77
Ungu77
hugo99
medan123
zodiaktoto
papua168
mansion88
luck99
asean188
rajazeus138
seru78
kampung99
Target99
gas123
coca4d
dinastibet
sultanbet188
Alamtoto
pwktoto pwktoto
rajagaming-52
rajagaming-53
rajagaming-54
rajagaming-55
rajagaming-56
rajagaming-57
rajagaming-58
rajagaming-59
rajagaming-6
rajagaming-60
rajagaming-61
rajagaming-62
rajagaming-63
rajagaming-64
rajagaming-65
rajagaming-66
rajagaming-67
rajagaming-68
rajagaming-69
rajagaming-7
rajagaming-70
rajagaming-71
rajagaming-72
rajagaming-73
rajagaming-74
rajagaming-75
rajagaming-76
rajagaming-77
rajagaming-78
rajagaming-79
rajagaming-8
rajagaming-80
rajagaming-81
rajagaming-82
rajagaming-83
rajagaming-84
rajagaming-85
rajagaming-86
rajagaming-87
rajagaming-88
rajagaming-89
rajagaming-9
rajagaming-90
rajagaming-91
rajagaming-92
rajagaming-93
rajagaming-94
rajagaming-95
rajagaming-96
rajagaming-97
rajagaming-98
rajagaming-99
sibayak99
triadtotogroup
nagatoto88
garwa4d
Kirintoto
triadsgp
triadsyd
triadjitu
triadmacau
triadtoto
triadtogel
triad4d
triadhk
torpedo99
scatter99
boom138
bosslot138
sibayak99
emas69
triad303
triadslot
pwktoto
triadtogel
triadhk
nagatoto88
garwa4d
torpedo4d
triadmacau
triadtoto
triadmacau
triadtoto
triadtogel
triadhk
scatter99
sibayak99
emas69
triadjitu
emas69
scatter99
sibayak99
boom138
pwktoto
torpedo4d
torpedo4d
torpedo4d
torpedo4d
nagatoto88
nagatoto88
nagatoto88
garwa4d
garwa4d
garwa4d
triadtoto
triadtoto
triadtoto
triadtogel
triadtogel
triadtogel
triad4d
triad4d
triad4d
triad4d
triad4d
triad4d
triadhk
triadhk
triadhk
triadhk
triadhk
triadhk
triadmacau
triadmacau
triadjitu
triadjitu
triadjitu
scatter99
scatter99
scatter99
scatter99
scatter99
sibayak99
sibayak99
sibayak99
sibayak99
sibayak99
sibayak99
sibayak99
sibayak99
boom138
emas69
emas69
rokettoto
rokettoto
rokettoto
rokettoto
bukitdita
kirintoto
kirintoto
triadsgp
triadsgp
triadsyd
triadsyd
torpedo99
torpedo99
torpedo99
torpedo99
premium138
premium138
premium138
premium138
premium138
premium138
bosslot138
bosslot138
bosslot
bosslot138
bosslot138
pusat69
pusat69
dompet69
dompet69
dompet69
dompet138
dompet188
dompet168
dompet123
harta69
triadslot
triadslot
triad303
138vip
138vip
triadtogel
triadtoto
triad4d
triadhk
triadhk
triad4d
triadtogel
triadjitu
triadmacau
boom138
garwa4d
scatter99
emas69
torpedo4d
nagatoto88
vinaslot
vinaslot
vinaslot
pwktoto
holyslot123
Amanah99
Rupiah777
horastogel
cuanslot
okta138
tango168
lotus777
bostoto138
medali69
milojitu
Lotre78
lux77
Gorilatoto
Hoki338
Dewapoker77
baikbet
sule78
lavatoto
uang138
Merak99
porto4d
hemattoto
Kaca138
puri138
anginbet
Joglo4d
juragantogel
Mahyong69
sojubet
sakti777
StarJoker69
grab78
spacetogel
jarum169
Kudatoto
pangkalanbet
ten88
opera99
satelit69
koin88
pondok338
jaring338
pubtogel
milo338
thor388
deltatoto
bdjitu
mirana99
amat123
autobet123
Shio77
gemoy188
planet888
Maria99
makmurwin
pakdejp
geber777
lato777
Melatibet
bankslot
hujantogel
coco69
Rusa69
Apollo303
sule777
namabet
Mars77
moon138
Pancingslot
Pulaubet
rumah88
cumi303
prada68
versace138
Koala4d
lobby69
lux78
usaha4d
kambingtogel
Musangtoto
delta777
Jeweltoto
pos188
lava77
maluku303
kompor88
luckslot
Lotre169
lotus68
raffi169
tambang388
ratuzeusqq
dinasti99
Modalhoki108
asiajitu
judi78
astra78
partaiqq
rumah69
Meriam123
evosbet88
Sayangbet
Lilin4d
Cemaraslot
furla69
kumis4d
Bandungslot
japan78
hokislot123
hulk303
Pragmatic69
chivas69
krisna188
Lyonslot
ASIABET168
topislot
bola123
ultra365
ios55
kompor77
sinaga138
kelapabet
padang777
Rajawin777
Jakarta88slot
Becak168
babetogel
primaslot
Moonslot
palu338
pulautogel
botaktogel
platinum138
cici169
gunturtogel
Kacang4d
dewabet138
spin388
homebet69
bursatoto
mami4d
pasbet
aduhoki
lava69
pagoda388
meledak99
dalang138
Gama188
dino777
papua338
darat123
hokiwin55
Cobra777
Merak88
crown78
preman77
grab188
terminal388
apiwin
madura78
sinar303
Dupawin
Santuy188
kera388
Modalhoki68
omuslot
Peri123
divabet
macau388
Angsa138
keris69
DOMINOPKV
Bos69
Sawitjitu
jaring99
layar77
tayototo
taro168
pejuang388
next88
harapan168
hemat123
Shio88
apidewa77
parisjp
pohon69
Lotre777
taruna123
asean168
giga69
StarJoker123
tempat99
Sisir4d
Tokek78
bosstogel
pakdeslot88
wisslot
rumah108
dominoslot
cola123
jili88
kompas77
bisnis77
kungfu69
Arjuna77
sensa123
Piramida4d
gacor365
pucuk777
Lotre123
wayang777
Gama178
WLA88
langitmpo
Robot4d
kumbang123
Logam4d
Sawit138
Bca168
petir88
tokyobet
tempo123
Permen178
Gacorbos99
wiratogel
LUNAS805
sateslot
barbar188
maxwin123
pecahtogel
Menang77
demotogel
trisula4d
candy138
bostoto188
demo388
citatogel
SIRKUIT138
Boy4d
Kalaslot
formulabet
Kode99
icon55
domino123
cartel303
jingga4d
Luxuryqq
space168
Legenda4d
porto169
api69
ASIAMPO77
wiki69
fasslot
cincin77
rajatoto68
Merak78
batastogel
gem108
buku99
furlabet
versace168
Sayang777
marvel365
kumis138
sushitoto
cbototo
latar77
Hadiah4d
solusi138
udara4d
sayang188
maha777
milo55
taro303
Dunia88
sejuta188
Dewapokertogel
Luxurygg
KOBOYPOKER
Aksara77
amat303
unggul123
oris77
kingdomjitu
merci4d
Aontoto
gemoyslot
geloratoto
layar69
winning138
sobet78
klik303
gilagg
bantamtoto
Sbo4d
Tombol4d
maya303
spin6d
sumo123
lambe88
barbar88
kadobet168
solid169
oasis365
karo303
duta69
sumo88
Pandawa123
ipar777
bengkelslot
macanslot
abc69
judolbetqq
Laku123
obor77
Lampion4d
memori77
jepang169
plntoto
ASIAPKV
Duyung88
Hijau123
dewanslot
MAXWIN888
SUARABET77
empirebet
Kucingtoto
kakek138
idr188
coca123
sisri77
jamu123
cumi99
fire123
persentogel
moon4d
dutabet
jaring365
Bigwin178
Gacorbos169
toto388
evosgamingg
kado99
WLA55
kadal303
rumah168
Poker138
Aztectoto
gasing78
extrabet
urban168
Topengslot
planet388
Angkatoto77
mulia88
qq69
luck388
epictogel
GACORBOS
icon169
atlas169
bentototo
jamu4d
libas169
holiday69
hulk77
skor77
karo168
colekbet
Bendera99
suhu4d
Dayak123
radentogel
KOBOY888
memori108
lajubet888
JUARAWIN88
BIMO77
jokerbetqq
AREASLOTO
juara77
dewi138
DEWIBET777
nusapoker
jilibet
Ikan303
kadalslot
depototo
harum123
pawang88
krisna123
madu55
Khusustogel
taktik388
Wahana4d
ovo168
mesinslot
Gogo90
bromo99
Badutjitu
Mega777
sentosa69
kamus168
Tigerslot
tempatslot
wazebet
sekai777
airtogel
Agen99
colek777
pasang388
pigi388
Angkatoto123
batam69
kudetabet69
mewah123
fuji338
papua78
murahpoker
cincin365
memori69
hantu78
anak777
Kapten99
Nanas188
Glory77
wiki78
PEDANGBET
mahjongs138
ipar78
motoslot88
POV99
bingo4d
ratuslot777
YUPI188
ASIASLOT888
fire777
pasti138
batam777
julietslot
iklan88
kamus77
sobet99
capital99
Sicbo4d
paris4d
daya365
amat168
roslot55
Kaktusslot
cakra123
Abu123
krisna77
guntur365
PEDANGJITU
panca123
Kodok123
ASIAKING777
JPSLOT168
wuling88
kaya77
KOBOIBOLA
garpu777
kingbet169
pir69
extra188
oren77
cair365
kingdomjp
dewaslot138
nagapoker777
cici138
Daun777
surga6d
holyslottoto
jakarta303
dinasti777
suara78
Mbah4d
HOKIOM88
zona77
unggul169
tempat123
Arus138
retro388
mampirtoto
sulaptogel
nagawin168
pecah188
bangsa338
ASIAHOKI88
neopoker
mesin188
canduslot777
dino78
asus88
Mangga4d
kumistogel
nama88
kkslot55
LUNA999
Tokcer69
Logam303
kkslot108
lgo188
gemoy777
ultra99
tahunslot
ligajp88
kampusslot
babe69
macau128
taktik123
kado338
Angsa77
latarslot
juliet777
lavaslot
suburbet
doyan77
ladang77
Dupaslot
YUPIBET
AREA188
betagg
usaha169
AREAWIN88
megawinbet
Tokcer168
mandiri99
MANTAP138
mahal99
Gobertogel
abc77
mulia99
bonus303
kembar388
sensatogel
atom188
gebyar77
baik388
balon138
Master77
ovo338
gaco169
edanbet
pistolslot
air169
kembang169
dna303
wigo123
ladangslot
pasang338
suryatogel
DOMINOBET77
kembar188
diva388
pohonjitu
Sakuraqq
kumis168
ASIATOTO777
Premium188
rupiah4d
CERIAPOKER
KAYA78
kebunbet
sawi69
pub365
pesiar69
Wild777
Tores777
paus168
bom108
Dollarjitu
vegas77
wis338
Kancil69
angkasaslot
Dolan138
semangat303
jaritogel
daun69
nova123
darat303
SERUBET88
selat123
hantu88
serbatoto
balon123
tenbet
padi78
benuawin
Sensa188
Emas88
Rajawalitogel
musangtogel
sarana78
sugar365
lexus108
bom123
kso123
luck4d
puncak88
vista123
muara69
Rutantoto
ceria88
RAFI777
alasbet
durentoto
mpomaster
cipitbet
usaha138
leobet
mantra168
Akun188
Nanastogel
alexa88
Tombol168
slotbom68
solid78
gunturslot
sake138
Gloryslot
luck77
raksasa138
mildbet
Doku123
Yakuza777
bostoto77
jutawan168
odin123
lampu168
cumi168
mega169
puri188
petatogel
dadu168
mahadewa168
karirtogel
istana88
serbu123
kumbang99
pulau169
Sarangslot88
muliaslot
tiktoktoto
retro4d
ayo68
Dugem88
jepe338
bns99
leo303
turbo77
timur77
baiktogel
masterbet123
Mansionslot
petirslot
retro69
unggul168
POV69
musik168
kapaljudi777
Habanero138
marvel188
kejubet
ios99
Ninjaslot
permen169
fix338
koi138
madura168
gerbang338
desa77
sushi168
Ikanslot
opera123
oren365
luckbet
Rusa77
Ungu77
hugo99
medan123
zodiaktoto
papua168
mansion88
luck99
asean188
rajazeus138
seru78
kampung99
Target99
gas123
coca4d
dinastibet
sultanbet188
Alamtoto
pwktoto pwktoto
rajagaming-52
rajagaming-53
rajagaming-54
rajagaming-55
rajagaming-56
rajagaming-57
rajagaming-58
rajagaming-59
rajagaming-6
rajagaming-60
rajagaming-61
rajagaming-62
rajagaming-63
rajagaming-64
rajagaming-65
rajagaming-66
rajagaming-67
rajagaming-68
rajagaming-69
rajagaming-7
rajagaming-70
rajagaming-71
rajagaming-72
rajagaming-73
rajagaming-74
rajagaming-75
rajagaming-76
rajagaming-77
rajagaming-78
rajagaming-79
rajagaming-8
rajagaming-80
rajagaming-81
rajagaming-82
rajagaming-83
rajagaming-84
rajagaming-85
rajagaming-86
rajagaming-87
rajagaming-88
rajagaming-89
rajagaming-9
rajagaming-90
rajagaming-91
rajagaming-92
rajagaming-93
rajagaming-94
rajagaming-95
rajagaming-96
rajagaming-97
rajagaming-98
rajagaming-99
sibayak99
triadtotogroup
nagatoto88
garwa4d
Kirintoto
triadsgp
triadsyd
triadjitu
triadmacau
triadtoto
triadtogel
triad4d
triadhk
torpedo99
scatter99
boom138
bosslot138
sibayak99
emas69
triad303
triadslot
pwktoto
triadtogel
triadhk
nagatoto88
garwa4d
torpedo4d
triadmacau
triadtoto
triadmacau
triadtoto
triadtogel
triadhk
scatter99
sibayak99
emas69
triadjitu
emas69
scatter99
sibayak99
boom138
pwktoto
torpedo4d
torpedo4d
torpedo4d
torpedo4d
nagatoto88
nagatoto88
nagatoto88
garwa4d
garwa4d
garwa4d
triadtoto
triadtoto
triadtoto
triadtogel
triadtogel
triadtogel
triad4d
triad4d
triad4d
triad4d
triad4d
triad4d
triadhk
triadhk
triadhk
triadhk
triadhk
triadhk
triadmacau
triadmacau
triadjitu
triadjitu
triadjitu
scatter99
scatter99
scatter99
scatter99
scatter99
sibayak99
sibayak99
sibayak99
sibayak99
sibayak99
sibayak99
sibayak99
sibayak99
boom138
emas69
emas69
rokettoto
rokettoto
rokettoto
rokettoto
bukitdita
kirintoto
kirintoto
triadsgp
triadsgp
triadsyd
triadsyd
torpedo99
torpedo99
torpedo99
torpedo99
premium138
premium138
premium138
premium138
premium138
premium138
bosslot138
bosslot138
bosslot
bosslot138
bosslot138
pusat69
pusat69
dompet69
dompet69
dompet69
dompet138
dompet188
dompet168
dompet123
harta69
triadslot
triadslot
triad303
138vip
138vip
triadtogel
triadtoto
triad4d
triadhk
triadhk
triad4d
triadtogel
triadjitu
triadmacau
boom138
garwa4d
scatter99
emas69
torpedo4d
nagatoto88
vinaslot
vinaslot
vinaslot
pwktoto

Growth Modulation in Children for Angular Deformity Correction around knee – Use of Eight Plate
Vol 1 | Issue 1 | July-Sep 2015 | page: 33-37 | Sandeep Patwardhan, Kunal Shah, Ashok K Shyam, Parag Sancheti.
Authors : Sandeep Patwardhan[1], Kunal Shah[1], Ashok K Shyam[1], Parag Sancheti[1].
[1] Sancheti Institute for Orthopaedics and Rehabilitation 16, Shivajinagar, Pune, India.
Address of Correspondence
Dr. Kunal Shah
Sancheti Institute for orthopaedics and Rehabilitation
16, Shivajinagar, Pune, India.
Email-orthokunal@yahoo.com
Abstract
Background: Angular deformities around the knee joint in skeletally immature children are treated with methods of reversible hemiepiphysiodesis like staples, transphyseal screw and eight plate. Hemiepiphysiodesis using Eight plate has showed good results with advantage being faster correction, less complications and can be used in younger age.
Methods: The aim of this retrospective study is show the efficacy of eight plate application and its complication rate. Nineteen patients (37 physes) (unilateral: 3; bilateral: 16) with angular deformity were treated with eightplate application. Seven with pathological physes and twelve with idiopathic physes. Outcome assessment was done clinically with calculation of intermalleolar /intercondylar distance and radiologicaaly with mechanical and anatomical axis. Correction achieved was considered when anatomical/mechanical axis were within normal limits and intermalleolar/intercondylar distance was less than 5 cm.
Results: The average age of intervention was 7.4±2.96 years (range 2.4 -11.2years). Rate of correction of IMD/ICD was 1.14 cm per month. Rate of correction of mechanical axis was 0.76 o per month. Rate of correction of anatomical axis was 1.04o per month. The average duration of eight plate removal 12.4 months (range 7-24 months).There were two complications one patient with screw backout and other with overcorrection.
Conclusion: Reversible hemiepiphysiodesis using eight plate is and effective method with minimal complications and faster rates of correction. Idiopathic physes show faster rates of correction than pathological physes. Physeal growth arrest is not seen with eight plate application. Larger data and long term follow up is required to assess the rebound deformity after eight plate removal.
Keywords: Reversible, hemiepiphysiodesis, angular deformity, eight plate.
Introduction
Pathological angular deformities of knee are common childhood deformities. Majority of them are idiopathic while others are due to some local or systemic cause [1].They present with cosmetic deformity, mild discomfort, gait disturbance, joint instability and limitation of activities or symptoms of causative disease. More importantly they predispose to early arthritic changes in the knee joint and secondary changes in hip and ankle joint [2, 3].Therefore it is important to identify them early and treat accordingly. Treatment depends mainly on cause of disease, age of child and amount of deformity. Corrective osteotomies once considered gold standard[3], are no longer advised in skeletally immature child, unless acute correction is required[4] or deformity is severe (>30o)[1]. Distraction osteogenesis using external fixator was used for gradual growth arrest, but it had several disadvantages like poor compliance, pin tract infections and longer time required to achieve correction [1].
Epiphysiodesis has emerged as the treatment of choice for angular deformity correction in skeletally immature patient with mild to moderate deformity[1,5]. Historically many methods for permanent and temporary epiphysiodesis were described [1]. Permanent methods depended on accurate timing of intervention to prevent overcorrection or under correction[5]. But none of the current methods of determining bone age are reliable [6, 7].Therefore reversible methods of epiphysiodesis have become the mainstay of treatment. It involves mainly staples, transphyseal screws and recently eight-plate has been used. Hemiepiphysiodesis with staples pose problems like migration, breakage and bending of implant, physeal growth arrest and rebound deformity[8].Transphyseal screws have shown fewer complications with implant and rebound phenomenon is less as compared to staples[5].However its reversibility is doubted by many as it cross the Physis[9,10]. Use of eight plate has shown promising results with fewer complications, faster correction and reversible growth [11, 12] yet literature is still sparse on use of this device. The purpose of this prospective study is to show the efficacy of hemiepiphysiodesis using eight-plate in correction of angular deformities around knee.
Material and Method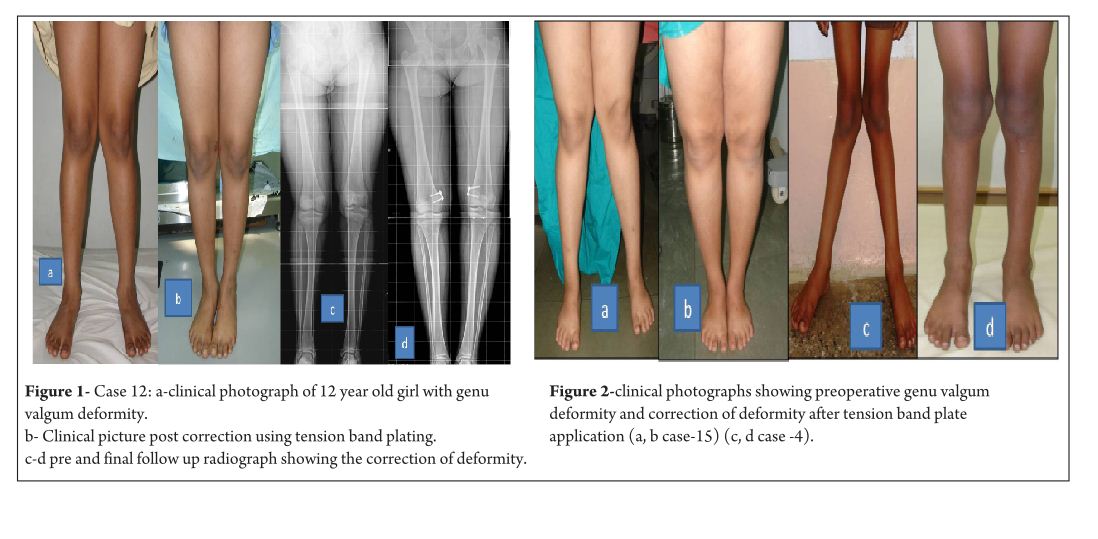
This is a retrospective study of 19 patients (37physes, 16 bilateral and 3 unilateral) with symptomatic angular deformity treated with 8 plate application. Out of the 19 patients there were 9 boys and 10 girls. Cause of angular deformity was rickets in 4, Down’s syndrome in 1, post septic in 1, skeletal dysplasia in 1 and idiopathic in 12. Genu varum was seen in 5 patients (8 physes) and genu valgum was seen in 14patients (29 physes).17 patients had 8 plate application in distal femoral physis, 1 patient had in proximal tibia and 1 patient had in both femur and tibia. Plates were applied in both tibia and femur to achieve faster rate of correction [11]. Surgical treatment was given to patients who were symptomatic or asymptomatic patients with age more than 4 years, with intermalleolar/intercondylar distance (IMD/ICD) more than 10 cm and/or mechanical axis more than 3° (valgum/varum). Contraindications to surgery included limbs with physiologic deformity, physeal arrest and maturity. Physiologic deformities were defined as genu varum in less than 2 years and genu valgum quantified by tibio-femoral angle less than 8° or IMD of less than 8 cm in age less than 4 years[14]. Physeal bar was defined as bony connection across physis, potentially affecting physeal growth [15]. The upper limit of age for surgical correction was at least one year of growth remaining [7, 9] as assessed on carpal age. In patient nearing skeletal maturity, hand film was taken to quantify amount of growth remaining. Standing lower limb scanogram with patella facing anteriorly [16] was taken preoperatively and at final follow up to look for mechanical axis and anatomical axis. Radiographically, mechanical axis of lower limb was measured as angle between mechanical axis of femur (centre of femoral head to centre of knee joint) and mechanical axis of tibia (centre of knee joint to centre of ankle mortise).The centre of knee joint was used to determine the mechanical axis [9]. The normal mechanical axis was considered as 0±3°[13]. With radiolucency of the physis it was difficult to define the centre of the knee joint and in such cases the centre of the distal physis of femur and proximal physis of tibia were considered in measurement. Tibiofemoral angle was measured as angle between long axis of femur and long axis of tibia. Normal was considered as 6° [16].
Clinically, intermalleolar and intercondylar distance were measured with patient in standing position with both patella facing forwards and medial malleolus/medial condyles just touching each other both preoperatively and at final follow up. Preoperative data was collected from the patient’s hospital records and from the surgeons own database. All patients with rickets were treated with appropriate medical management. Correction was considered when mechanical axis/anatomical axis were corrected and IMD/ICD was less than 5cm.
Surgical technique
With patient in supine position, tourniquet was applied to achieve haemostasis. Centre of Physis was marked using k wire under fluoroscopy guidance. Incision is taken and dissection done to reach the periosteum taking care that the periosteum is not breached and perichondrial blood supply is maintained. Plate inserted over the K wire and position confirmed under image intensifier, cannulated screws inserted parallel to Physis. Screw position checked under image intensifier in both antero-posterior and lateral view. Closure done and dressing applied. Postoperatively no immobilisation was required and patients were mobilised full weight bearing as tolerated from post op day 1. No walking support was required. Patients were followed up prospectively at every 3 month and knee radiographs were taken antero-posterior and lateral view to look for screw divergence and clinically IMD/ICD was measured.
Results
The average age of intervention was 7.4±2.96 years (range 2.4 -11.2years).The mean values of mechanical axis, tibiofemoral axis, IMD/ICD and duration of correction were calculated excluding the patient with overcorrection [case no 19] to avoid wide deviation from mean values. The mean preoperative IMD/ICD was 15.8cm ± 3.96 (range 10 cm to 22 cm) .The mean correction 1.6cm ± (range 0cm to 4 cm). Rate of correction was 1.14 cm per month. The mean preoperative mechanical axis was 13.4o± 5 (range7o to 25o).The mean post operative mechanical axis was 3.9o ±2.44 (range 0o to 10o). Rate of correction was 0.76 o per month .The mean preoperative tibiofemoral angle was 18.7o ±5.1 (range 7o -28o). The mean post operative tibiofemoral angle was 5.8o ± 2.29 (range 0o -12o). Rate of correction was 1.04o per month .Rate of correction in idiopathic and pathological physis group are depicted in table 1 and 2).The average duration of eight plate removal was 12.4 months (range 7-24 months). It was 13.3 months in pathological group and 11.8 months in idiopathic group. Figure 1 shows clinical and radiological correction in terms of IMD/ICD, mechanical axis and tibiofemoral axis. One patient was excluded from the data, a case of pathological genu valgum because the physis became fused before correction was achieved .The patient was treated with corrective osteotomy. Thus, emphasizing on preoperative planning in terms of age of intervention and aetiology deformity. There were two complications; one patient had screw back out which was revised. Other patient had reversal of deformity from 24° valgus to 22° varus due to delayed follow up [case 19]. She was treated with removal of 8 plate and is currently under observation for spontaneous correction. None of the patient had limb length discrepancy except (case 12) had 3 cm femoral shortening. Clinical data and outcome assessment in idiopathic and pathological group are depicted in table 1 and table 2.
Discussion
Physeal growth in child depends on variety of factors like biomechanical, hormonal and genetic [17]. Growth modulation using eight-plate depends on biomechanical growth modification based on Hueter-volkmann principle. Sustained compression parallel to physis leads to growth retardation and subsequent correction of deformity [9]. Eight-plate functions as flexible device which produces sustained compression at physis. The compression is not constant as the screws diverge with correction and with maximum divergence the plate bends, hence also called as tension band plate [11]. Eight-plate serves as non rigid implant with lateralisation of fulcrum for deformity correction. Thus, leading to faster rates of correction [ 2, 8]. Staples and transphyseal screws are rigid implants with centralised fulcrum for deformity correction [13]. They produce constant compression at physis. Thus they take longer time for deformity correction [2, 8]. Staples and transphyseal screws are rigid implants and if a prolonged duration is required for correction of deformity, they may cause physeal arrest [17]. In contrast eight plates are relatively flexible implants as it allows for screw separation. This is one of the reasons for decreased incidence of physeal arrest and makes it safer to use in younger children when compared to staples. In our study, three patients below the age of 3 years were treated successfully without any complications [case no 2, 7 and 11]. Clinical assessment of growth modulation by using IMD/ICD is reported for studies using staples [18] but not in studies using eight-plate. Since IMD/ICD was the major criteria to define the indication for surgery in our series, we have used the same as the primary outcome measure. We believe that IMD/ICD is an important clinical measure as majority of our patient were asymptomatic with cosmetic deformity and follow up parent counselling was easier. However standard values for particular age and race vary [14, 19].There can also be high rate of inter observer discrepancy and this is one of the limitations of the study. Radiographic measurements are used as outcome measures in papers on growth modulation using eight-plate like tibio-femoral axis, mechanical axis, joint orientation angles, mechanical axis deviation , articular –diaphyseal etc[2,10,11,20]We have used two radiological outcome measures, the hip knee ankle mechanical axis and the tibio-femoral angle. In our study we found that tibiofemoral angle and mechanical axis improved significantly. Standard antero-posterior and lateral radiographs of knee joint are useful in follow ups to see the effect of epiphysiodesis as seen with screw divergence. Joint orientation angles were not used, as scanograms become distorted due to magnification and parallax leading to false values[6].Also in young children it is difficult to visualise the distal femur and proximal tibia epiphyseal contours to accurately mark these angles. Ballal et al [11] showed that mean rate of correction of tibiofemoral axis 0.7°/month for distal femur and 0.5°/month in proximal tibia. Burghardt et al [20] showed mechanical axis correction of 1.73mm/month. In our study mean rate of correction of mechanical axis was 0.76°/month and tibio-femoral axis was 1.04°/month.
Rate of correction is faster in children less than 10 years as shown in study by Ballal et al [11]. In our study, due to smaller sample size of patients more than 10 years of age we could not assess this in our series. We did compared the rate of correction between the idiopathic and pathological group with former showing faster correction (Table 3 and 4). This corroborated with findings of Boero et al.No difference in rate of correction was encountered in terms of gender and type of deformity in our series. In our study two complications occurred, one patient had a screw back out (figure 3a) at 4 month after insertion, which was treated with revision of screw. However the rate of deformity correction was consistent with other patients in idiopathic physis group. We believe that the reason for back out may be placement of screw near the posterior cortex. Similar complications of screw loosening were seen in studies by Burghardt (n=1) [20] and Stevens (n=1) [2]. Other complication of overcorrection of deformity (figure 3b) was seen in one patient because of delayed follow up. This is justified as principally the sustained compression at physis will produce dynamic changes. Ballal et al [11] encountered one case of both screw and plate migration which was revised, such complication didn’t occur in our series. Several series encounter rebound growth after plate removal [2, 11, 20], we have not seen rebound of deformity in our patient with longest follow up of 2 years after plate removal. Complications related to implant like migration, breakage, bending of implants etc seen with staples are less common with eight -plate. Most dreaded complication of physeal arrest is not reported in our and other series [2, 3, 7, 10, 11, 20]. The threaded screws are less likely to extrude, especially in cartilaginous physis seen in younger age [8]. Screws are placed extra-periosteal and perichondrial blood supply is not hampered, so the chances of physeal arrest while insertion and removal are very less. Our study has drawbacks of small sample size and retrospective study design. However it does gives important inferences in terms of ability of 8 plates to correct the deformity and more importantly with minimal complications. However larger sample comparative studies will be required to establish the superiority of this method compared to other methods. Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
References
1. Celestre PC, Bowen RE. Correction of angular deformities in children- Current Orthopaedic Practice. 2009;20(6):641-647.
2. Stevens PM. Guided growth for angular correction: a preliminary series using a tension band plate. J Pediatr Orthop. 2007 Apr-May; 27(3):253-9.
3. Wiemann JM 4th, Tryon C, Szalay EA. Physeal stapling versus 8-plate hemiepiphysiodesis for guided correction of angular deformity about the knee. J Pediatr Orthop. 2009 Jul-Aug; 29(5):481-5.
4. Cho TJ, Choi IH, Chung CY, Yoo WJ, Park MS, Lee DY. Hemiepiphyseal stapling for angular deformity correction around the knee joint in children with multiple epiphyseal dysplasia. J Pediatr Orthop. 2009 Jan-Feb; 29(1):52-6.
5. Ghanem I, Karam JA, Widmann RF. Surgical epiphysiodesis indications and techniques: update. Curr Opin Pediatr. 2011 Feb; 23(1):53-9.
6. Friend L, Widmann RF. Advances in management of limb length discrepancy and lower limb deformity. Curr Opin Pediatr. 2008 Feb; 20(1):46-51.
7. Burghardt RD, Herzenberg JE, Standard SC, Paley D. Temporary hemiepiphyseal arrest using a screw and plate device to treat knee and ankle deformities in children: a preliminary report. J Child Orthop. 2008 Jun; 2(3):187-97.
8. Eastwood DM, Sanghrajka AP. Guided growth: recent advances in a deep-rooted concept. J Bone Joint Surg Br. 2011 Jan; 93(1):12-8.
9. Stevens PM. Guided growth of the lower extremities. Current Orthopaedic Practice. March/April 2011; 22(2):142–149
10. Schroerlucke S, Bertrand S, Clapp J, Bundy J, Gregg FO. Failure of Orthofix eight-Plate for the treatment of Blount disease. J Pediatr Orthop. 2009 Jan-Feb; 29(1):57-60.
11. Ballal MS, Bruce CE, Nayagam S. Correcting genu varum and genu valgum in children by guided growth: temporary hemiepiphysiodesis using tension band plates. J Bone Joint Surg Br. 2010 Feb; 92(2):273-6.
12. Stevens PM, Klatt JB. Guided growth for pathological physes: radiographic improvement during realignment. J Pediatr Orthop. 2008 Sep; 28(6):632-9.
13. DeBrauwer V, Moens P. Temporary hemiepiphysiodesis for idiopathic genuavalga in adolescents: percutaneous transphyseal screws (PETS) versus stapling. J Pediatr Orthop. 2008 Jul-Aug; 28(5):549-54.
14. Heath CH, Staheli LT. Normal limits of knee angle in white children–genu varum and genu valgum. J Pediatr Orthop. Mar-Apr 1993.
15.Paterson HA Epiphyseal growth plate fracture. Springer, Berlin 2007.
16. Paley D. Principles of Deformity Correction. Berlin, Germany: Springer; 2002.
17. Frost HM, Schönau E. On longitudinal bone growth, short stature, and related matters: insights about cartilage physiology from the Utah paradigm. J Pediatr Endocrinol Metab. 2001 May; 14(5):481-96.
18. Courvoisier A, Eid A, Merloz P. Epiphyseal stapling of the proximal tibia for idiopathic genu valgum. J Child Orthop. 2009 Jun; 3(3):217-21.
19. Omololu B, Tella A, Ogunlade SO, Adeyemo AA, Adebisi A, Alonge TO, Salawu SA, Akinpelu AO. Normal values of knee angle, intercondylar and intermalleolar distances in Nigerian children. West Afr J Med. 2003 Dec; 22(4):301-4.
20. Burghardt RD, Herzenberg JE. Temporary hemiepiphysiodesis with the eight-Plate for angular deformities: mid-term results. J Orthop Sci. 2010 Sep; 15(5):699-704.
21. Boero S, Michelis MB, Riganti S. Use of the eight-Plate for angular correction of knee deformities due to idiopathic and pathologic physis: initiating treatment according to etiology-J Child Orthop 2011;5(3):209-216.
(Abstract) (Full Text HTML) (Download PDF)
Apophyseal Metaphyseal combination injury to Olecranon in a healthy Adolescent – A rare injury and review of literature
Vol 1 | Issue 1 | July-Sep 2015 | page:51-53 | Ganesh Singh Dharmshaktu, Anshuman Vijay Roy.
Authors : Ganesh Singh Dharmshaktu[1], Anshuman Vijay Roy[2].
[1] Department of Orthopaedics, Government Medical College, Haldwani , Uttarakhand.
[2] Department of Orthopaedics, Krishna Hospital and Research Centre, Haldwani , Uttarakhand.
Address of Correspondence
Dr. Ganesh Singh Dharmshaktu , Department of orthopaedics , Government Medical College , Haldwani ( Uttarakhand ) . PIN -263139. Email: drganeshortho@gmail.com
Abstract
Background: Apophyseal injuries of olecranon have limited number of case reports and series owing to its rarity. Pure apophyseal avulsions are very rare and so are apophyseal metaphyseal combination injuries. No guidelines exist for the uniformity of the treatment and various modalities have been tried in sporadic reports. A keen clinical observation is required to suspect the possibility of these injuries followed by good imaging confirmation. Concordance of associated disorders like osteogenesis imperfecta with such injuries underlines the importance of ruling out this clinical entity in such cases.
Keywords: Fracture, Apophysis, Olecranon, Injury. Tension band wiring.
Introduction
Upper extremity is common site of bony injuries in children with reported incidence of 65% to 75% in the literature. 7% to 9% of these injuries are elbow injuries.[1] Apophysis is a term usually applied to an epiphysis that is subjected to traction by muscle insertion and its physiological pull.[2] The injury to the region if displaced can cause serious morbidity and functional limitation and thus warrants appropriate treatment. Non operative management is limited to only undisplaced injuries while injuries with more than 3-5 mm. of displacement warrants open reduction followed by fixation with varying methods. Open reduction and compressive fixation has widely been tried successfully with various implants like screws, tension band wiring or resorbable sutures. There has not been significant growth related problem with compression forces as a result of internal fixation.[2]
Case Report
A 12 year old boy was presented to us with history of injury to his right elbow following fall from height two days back. He was taken to a local practitioner before coming to us with a make do splint of wooden sticks. There was swelling, pain and difficulty in using the affected limb. There was tenderness present and swelling more over the posterior aspect but no raised temperature and intact distal neurovascular status. There was no appreciable crepitus or frank abnormal mobility present and a proper elbow examination including range of motion status was limited by swelling and pain. The radiograph of the affected elbow showed an apophyseal-metaphyseal combination injury with displacement. The olecranon apophysis with a rim of metaphysis was avulsed. There was no associated injury present. There was neither any history of frequent or multiple bony injuries in the past related or remote to present condition nor presence of blue sclera or abnormal dentition. The parents of the boy were explained and advised operative intervention of the injury. Following an informed consent of parents in view of patient being minor and under aseptic precautions open reduction and internal fixation was planned and carried out.
Result
The open reduction and internal fixation was performed and secured with tension band wiring (TBW). The posterior approach was used to access the injury site, The avulsed part was provisionally reduced and held together with pointed clamps while TBW was carried out in standard manner using two parallel Kirschner’s wires and a wire loop in figure of eight fashion. The operation went uneventful and so was peri-operative period. The stitches were removed on tenth day and patient was advised supervised physiotherapy after two weeks. The follow up initially at three, six twelve weeks and then after three and six months were uncomplicated and the range of motion improved all this while. The final follow up at six months showed normal range of motion as compared to contra-lateral side. There was no problem with hardware in the follow up and those were removed subsequently after months.
Discussion
The type 3 injuries related to olecranon apophyses are complete fractures with type 3 (a) as pure avulsions and type 3(b) as apophyseal-metaphyseal combination injuries.[2] Type 3(b) injuries are commoner in older children while type 3(a) usually involves younger children. This pattern of injury has been likened to Salter-Harris type 2 injury.[3] Apophyseal injuries of olecranon are uncommon with limited reported incidents.[4] Most of these injuries have been associated with patients of osteogenesis imperfecta.[5] Osteognesis imperfecta cases ( like tarda form) show higher incidences for this injury.[6] Apart from the fact that olecranon apophyses fractures are reported in relation with 50% cases of osteogenesis imperfecta, there have been reportedly higher rates of complication such as refracture in them.[7] It has been advised that hardwares should be maintained even after union in cases of osteogenesis imperfect due to this risk.[5,7] The elbow has rich vascularity with extraosseus network as well as intraosseus one.[8,9] The undisplaced fractures are amenable to conservative treatment with plaster of paris slab or cast and fracture unite well if length, angulation and rotation is properly taken care of. The displaced fractures has been managed with tension band wiring in most instances with fair to excellent results.[3,7,10] Some authors have used trans- osseous suture fixation for the fractures with good results.[11] Use of absorbable wires as supplemental fixation have also been reported.[12] As most of these injuries occur in children near skeletal maturity, no significant growth related problem is seen as compressive fixation across physes. The presented case is an uncommon variant of apophyseal olecranon injury in a normal child managed satisfactorily with appropriate techniques.
References
1. Landin LA, Danielsson LG. Elbow fractures in children: an epidemiological analysis of 589 cases. Acta Orthop Scand 1986; 57:309.
2. Erickson M, Frick S. Fractures of the proximal radius and ulna.In Beaty JH, Kasser JR. editors. Rockwood and Wilkins Fractures in children 7th ed. Philadelphia: Lippincott Williams and Wilkins;2010: 427-431.
3. Granthan SA, Kiernan HA. Displaced olecranon fractures in children. J Trauma 1975;15197-204.
4. Carney JR, Fox D, Mazurek MT. Displaced apophyseal olecranon fracture in a healthy child. Mil Med. 2007;172(12):1225-7.
5. Zionts LE, Moon CN. Olecranon apophysis fractures in children with osteogenesis imperfecta revisited. J Pediatr Orthop.2002; 22(6):745-50.
6. Di Cesare PE, Sew-Hoy A, Krom W. Bilateral isolated olecranon fractures in an infant as presentation of osteogenesis imperfect. Orthopedics 1992; 15:741-743.
7. Gwynne-Jones DP. Displaced olecranon apophyseal fractures in children with osteogenesis imperfecta. J Pediatr Orthop. 2005; 25(2):154-7.
8. Wilson PD. Fractures and dislocations in the region of elbow. Surg Gynecol Obstet 1933;56:335-359.
9. Haraldsson S. The intraosseous vasculature of the distal end of humerus with special reference to capitellum. Acta Orthop Scand 1957;27:81-93.
10. Poland J. A Practical Treatise on Traumatic Separation of the Epiphyses. London; Smith, Elder & Co, 1898.
11. Rath NK, Carpenter EC, Thomas DP. Traumatic pediatric olecranon injury: a report of suture fixation and review of the literature. Pediatric emergency care 2011; 27(12):1167-9.
12. Gortzak Y,Mercado E, Atar D, et al. Pediatric olecranon fractures: open reduction and internal fixation with removable Kirschner wires and absorbable sutures. J Pediatr Orthop 2006;26:39-42 .
(Abstract) (Full Text HTML) (Download PDF)
Osteosynthesis in a 10 year old boy with Fracture neck of Femur, Infected Nonunion with Implants In-situ, Neck Resorption and Avascular Necrosis -A case report.
Vol 1 | Issue 1 | July-Sep 2015 | page:48-50 | EG Mohan Kumar, GM Yathish Kumar.
Authors : EG Mohan Kumar[1], GM Yathish Kumar[1].
[1] Department Of Orthopedic Surgery, KIMS Al Shifa Hospital, Perintalmanna, Kerala, India.
Address of Correspondence
Dr. EG Mohan Kumar
HOD Department Of Orthopedic Surgery, KIMS Al Shifa Hospital,
Perintalmanna, Kerala- 679322 India.
Email- orthomohan@rediffmail.com.
Abstract
Background: Non union fracture femoral neck is one of the common complication of intra capsular fracture neck of femur in children as well as in adults and it is the most challenging problem to treat if femoral head salvage is attempted. Other common complication is avascular necrosis (AVN) of the femoral head with most reported incidences being <15% (range 0% to 67%), which is similar to the complication rate with non-neglected femoral neck fractures. We are reporting a case of 10 year old boy who elsewhere underwent closed reduction and internal fixation with canulated cancellous screw for Delbert type III fracture neck of femur, which subsequently got infected with a draining sinus, non union and AVN of femoral head with complete absorption of the neck in 4 months time. We received the patient at that stage. He was managed by two stage surgery. Initially the implants were removed the screw tracks were curetted out and filled with antibiotic sponge. After the infection was eradicated osteosynthesis and neck reconstruction was done using fibular strut and cancellous grafts through modified Watson Jones approach and anterior capsulotomy . We avoided metal implants for fear of infection and so also a subtrochenteric osteotomy which require fixation. A hip spica cast was given for 6 weeks. The neck length was restored, vascularity restored and fracture united with an excellently functioning hip.
Keywords: Femur neck fracture, infection, osteosysnthesis.
Introduction
Fractures of the femoral neck in children are not common[1]. They represent fewer than 1% of all the paediatric fractures2. However, complications accompanying these fractures are frequent—specifically avascular necrosis, non union and early closure of the proximal physis of the femur—resulting in decrease of neck length and coxa vara. The incidence of non union varies from 7 to 10%, depending on the location of the fracture in the neck of femur[2,3,4]. Delbet was the first to describe the fractures of the femoral neck. He published the first classification in the French literature. Since then, Colonna[5] has quoted the Delbet classification, which is still accepted in all the literature regarding this subject, and Ratliff[6] has described the evaluation criteria of the results, based on the presence of pain, joint mobility and the child’s capacity to maintain a daily activity. Most of the articles in the literature support bone grafting and a valgus osteotomy with some sort of fixation[7]. Only few cases reported with non union neck of femur treated by fibular strut graft alone without fixation and osteotomy. We feel that our case was unique due to presence of infection which makes the situation complicated. Here, we report a case of paediatric femoral neck fracture which went in for all described complications like AVN, non union, infection and neck resorption which was managed successfully by staged surgery. In the first stage eradication of infection and in second stage osteosynthesis and neck length restoration was attempted.
Case Presentation
A 10 year old boy sustained fracture neck of right femur following fall from tree 4 months back(Fig.1) and was initially treated elsewhere by closed reduction and Canulated Cancellous Screw and K wire fixation(Fig.2), but osteosythesis was failed due to infection and poor fixation. He presented to us with non union, neck resorption, avascular necrosis of head of femur and infection with implants insitu(Fig.3). His WBC count(13000cells/cumm), ESR(40mmhg/hour) and CRP(110) were elevated. X-Ray showed loosening of implants with surrounding osteolysis and he was managed in two stages. Initially implants were removed, debridement was done, screw tracks were curetted out and antibiotic sponge was kept inside the tracks and was put on antibiotics(Fig.4). Once the infection got settled when CRP became normal after two months he was taken up for second stage surgery. He was treated by autologous fibular strut grafting and cancellous graft packing through Modified Watson Jones approach. Intra-operatively he was put on traction table, reduction and alignment was checked under C-ARM guidance(Fig.5), we could restore the length of neck with fibula graft under C-ARM guidance and cancellous gaft harvested from iliac crest was filled around fibula graft bridging fracture site through anterior capsulotomy(Fig.6,7). Patient was immobilized in hip spica cast for 6 weeks(Fig.8), POP was removed and X-ray taken .Gradually hip and knee were mobilized. He was reviewed every month with radiograph which showed good union of fracture and vascularity of the head of femur spontaneously improved(Fig.9,10). Made partial weight bearing with the support of walker at 3 months post op and gradually increased weight bearing. Fracture consolidated by 6 months. At present his fracture is completely united, vascularity of head of femur regained(Fig.10). He has got 1cm shortening of limb and patient is back to school walking without support without any pain. Since the proximal physis is fused he may develop an increase in the present limb length discrepancy which we plan to correct later.
Discussion
Fracture neck of femur in children is a rare injury and can lead to many complications. Nonunion and AVN are very common complication which is nearly equal in neglected and treated cases of fracture neck of femur[8].Infection further adds to challenge in treating these cases. We got chance to treat such a patient with failed osteosynthesis neck of femur with all known complication like infection, pseudoarthrosis, avascular necrosis and neck resorption. Investigation of nonunion of neck of femur should include TC,DC,ESR and CRP to rule out infection especially in failed osteosynthesis, MRI may be required if x-ray features are not conclusive of vascular status of head of femur. In the literature there are few articles about treating this challenging problem. All are supporting valgus osteotomy some sort of fixation, few are supporting fibular grafting and cancellous screw fixation[4,9], but all concerning situations without infection. We planned to tackle the infection first and go for osteosynthesis with bone grafting alone without osteotomy or use of any hardware for fixation, in view of the subsided infection. Fibular strut graft gave a very good structural support also helped us to maintain the neck length and cancellous graft helped in fracture healing and to some extent improve vascularity of femoral head which made him walk again. Patient may have LLD which is to be addressed at skeletal maturity.
Clinical Relevance
Although fracture neck of femur in children is a rare injury, complications are very common and challenging to treat. Thorough investigations are must before treating these complications of neck of femur fracture. Infection must be ruled out in failed osteosynthesis. In selected cases fibula strut grafting and cancellous grafting allow neck reconstruction and fracture healing without fixation in children. Initial immobilization with spica cast and close follow up and monitoring during post operative period is essential to achieve the goal.
References
1. Miller WE (1973) Fractures of the hip in children from birth to adolescence. Clin Orthop Relat Res 92:155–187 [PubMed]
2. Ratliff AHC (1962) Fractures of the neck of the femur in children. J Bone Joint Surg Br 44:528–542 [PubMed]
3. Chrestian P, Bollini G, Jacquemier M, Ramaherison P (1981) Fractures du col du femur de lénfant. Chir Pediatr 22:397–403 [PubMed]
4. Ratliff AHC (1970) Complications after fractures of the femoral neck in children and their treatment. J Bone Joint Surg Br 52:175–183 .
5. Delbet cited by Colonna PC (1929) Fractures of the neck of the femur in children. Am J Surg 6:793–797.
6. RatliffAHC (1962) Fractures of the neck of the femur in children. J Bone Joint Surg Br 44:528–542[PubMed]
7. Pedro F. Tucci Neto, Fernando Baldy dos Reis, José Laredo Filho, , Edison Noboru Fujiki,Henri Bensahel, and Carlo Milani; Nonunion of fractures of the femoral neck in children ;J Child Orthop. 2008 Mar; 2(2): 97–103.
8. Amit Roshan, , The Neglected Femoral Neck Fracture in Young Adults: Review of a Challenging Problem; Clin Med Res. 2008 May; 6(1): 33–39.
9. Nagi ON, Dhillon MS, Gill SS.Fibular osteosynthesis for delayed type II and type III femoral neck fractures in children.J Orthop Trauma. 1992;6(3):306-13.
10. Miller WE (1973) Fractures of the hip in children from birth to adolescence. Clin Orthop Relat Res 92:155–187 [PubMed]
11. Rang M (1983) Children’s fractures. 2nd edn. J B Lippincott, Philadelphia
12. Canale ST, Bourland WL (1977) Fracture of the neck of the femur and intertrochanteric region of the femur in children. J Bone Joint Surg Am 59:431–443 [PubMed]
13. Ingram AJ, Bachynski B (1953) Fractures of the hip in children. J Bone Joint Surg Am 35:867–886[PubMed]
14. Lam SF (1971) Fractures of the neck of the femur in children. J Bone Joint Surg Am 53:1165–1179[PubMed]
15. Forlin E, Guille BA, Kumar SJ, Rhee KJ (1992) Complications associated with fracture of the neck of the femur in children. J Pediatr Orthop 12:503–509 [PubMed]
16. Hughes LO, Beaty JH (1994) Fractures of the head and neck of the femur in children. J Bone Joint Surg Am 76:283–291 [PubMed]
17. Colonna PC (1928) Fracture of the neck of the femur in childhood. Ann Surg 88:902–907[PMC free article] [PubMed]
18. Weiner DS, O’dell HW (1969) Fractures of the hip in children. J Trauma 9:62–79 [PubMed]
19. Durbin FC (1959) Avascular necrosis complicating undisplaced fractures of the neck of the femur in children. J Bone Joint Surg Br 41:758–765 [PubMed]
20. McDougall A (1961) Fractures of the neck of the femur in childhood. J Bone Joint Surg Br 43:16–28
21. Ogden JA (1974) Changing patterns of proximal femoral vascularity. J Bone Joint Surg Am 56:941–50[PubMed]
22. Trueta J (1957) The normal vascular anatomy of the human femoral head during growth. J Bone Joint Surg Br 39:358–373 [PubMed]
23. Chung SMK (1976) The arterial supply of the developing proximal end of the human femur. J Bone J Surg Am 58:961–970 [PubMed]
24. Sotto-Hall R, Johnson LH, Johnson RA (1964) Variations in the intra-articular pressure of the hip joint in injury and disease. J Bone Joint Surg Am 46:509–516 [PubMed]
25. Drake JK, Meyers MH (1984) Intracapsular pressure and hemartrosis following femoral neck fracture. Clin Orthop Relat Res 182:172–175 [PubMed]
26. Pauwels F (1965) Biomechanics of the locomotor apparatus. English edn. Springer, New York
27. Touzet P, Rigault P, Padovani JP, Pouliquen JC, Mallet JF, Guyonvarch G (1979) Fractures of the neck of the femur in children. Rev Chir Orthop Reparatrice Appar Mot 65:341–349 [PubMed]
28. Trueta J (1968) Vascular pattern of the femoral head during growth. In: Studies of the development decay of the human frame, 2nd ed. J. B. Lippincott, Philadelphia.
(Abstract) (Full Text HTML) (Download PDF)
Open reductions of Paediatric Supracondylar Humerus Fractures- When, How and, Risks
Vol 1 | Issue 1 | July-Sep 2015 | page:16-18 | Ashish Ranade, Gauri Oka.
Authors : Ashish Ranade[1], Gauri Oka[1].
[1] Dept. of Orthopaedics, Deenanath Mangeshkar Hospital, Pune 411004.
Address of Correspondence
Dr Ashish Ranade
Dept. of Orthopaedics, Deenanath Mangeshkar Hospital, Pune 411004.
Email address:ashishranade@yahoo.com
Abstract
Supracondylar humerus fracture is one of the commonest fractures in pediatric elbow. Usually closed reduction and percutaneous pinning is the preferred treatment for most of the displaced fractures. Nowadays closed reduction and percutaneous pinning has become standard of care for majority of displaced supracondylar humerus fractures. Rarely, an open reduction via appropriate approach becomes necessary. Various types of approaches that have been described are anterior, posterior, medial, lateral, and combined approaches. There is ambiguity of information as to selection of approach for doing open reduction in a supracondylar humerus fracture. There is debate about timing of treatment, approach selection and indications for doing open reduction.1 In this article we discuss indications, various types of approaches with their pros and cons and risks involved in open reduction of supracondylar humerus fractures in children.
Keywords: Supracondylar humerus fracture, open reduction, surgical approach.
Introduction
Supracondylar humerus fracture (SHF) is one of the commonest fractures in pediatric elbow. Nowadays closed reduction and percutaneous pinning has become standard of care for majority of displaced supracondylar humerus fractures. Rarely, an open reduction via appropriate approach becomes necessary. Various types of approaches that have been described are anterior, posterior, medial, lateral, and combined approaches. There is ambiguity of information as to selection of approach for doing open reduction in a supracondylar humerus fracture. There is debate about timing of treatment, approach selection and indications for doing open reduction [1]. In this article we discuss indications, various types of approaches with their pros and cons and risks involved in open reduction of supracondylar humerus fractures in children.
Case Example
A 9 year old boy was referred for the treatment of left supracondylar humerus fracture. He had sustained an injury following fall from a tree 10 days ago and was put in an above elbow splint in his village. On examination, radial pulse was present and he was neurologically intact.
The elbow was grossly swollen and there was deep abrasion with blister formation along the elbow crease on the anterior aspect. (Figure 1) There was ecchymosis along anterior aspect of elbow. The radiographs showed posterolaterally displaced type III supracondylar humerus fracture (Figure 2). Under general anaesthesia, closed reduction was attempted. Satisfactory reduction could not be achieved by closed means. Hence, a decision was made to perform open reduction. Considering the anterior wound, combined medial and lateral approach was chosen. Initially, a medial incision was made and the bony spike of the proximal fragment was separated from the brachialis fibres and the median nerve. At this point, reduction was attempted again. In view of difficulty in getting a satisfactory alignment, a lateral incision was made and the interposing tissues were removed. Periosteum was found to be torn on both sides. (Figure 3)After achieving open reduction, the fracture was fixed with crossed k wires and maintained in an AE slab for 3 weeks(Figure 4). Postoperatively, the patient made uneventful recovery and the fracture healed well in a satisfactory position. The elbow had 5 degrees loss of terminal flexion.
Discussion
Open reduction has been indicated for fractures with vascular injuries, signs of compartment syndrome, failure of closed reduction to achieve satisfactory alignment, and for severe swelling interfering to achieve good reduction [2-7]. In present day scenario, the main indication is failure to achieve satisfactory reduction by closed methods. This could be because of several factors such as instability of the fracture or interposition of neurovascular bundle or brachialis muscle. The overall proportion of supracondylar humerus fractures needing open reduction varies between 3 to 46% based on various studies[2,8-10]. This rate varies between centres and some centres may prefer to do open reductions than using closed methods. Delayed presentation of the fracture is one of the most important factors while discussing open reduction for supracondylar humerus fractures[ 5].
There are several options available for approach selection. There is no clear superiority of one approach over another. Mazzini and co-authors have published a systematic review of literature pertaining to surgical approaches in the treatment of open reduction and pinning[11]. In this review, authors found high frequency of poor results in terms of functional outcomes with posterior approach. High frequency of excellent results was found with the lateral and medial approach and a high frequency of good results within the anterior approach group. A Canadian study sites buttonholing of the proximal fragment through the brachialis muscle and interposition of joint capsule or periosteum between fragments[12]. With the posterior approach , anterior structures such as brachialis, and the neurovascular bundle cannot be accessed and probably the posterior scar leads to limitation of movements of the elbow joint[13]. In the same article, authors have found the change in the carrying angle (cosmetic outcome) as the most common complication seen after an open reduction via the posterior or lateral approach. However, relatively newer studies utilizing posterior approach do not report these complications [7,14]. Medial column communition and internal rotation and/or varus tilt of the distal fragment may be addressed sufficiently through lateral/posterior approach. In review by Mazzini et al, the time to union remains the same irrespective of the approach used. There was higher tendency of ulnar nerve injury in the posterior and lateral approach group. This is attributed to lack of direct visalization of ulnar nerve. Based on the findings, authors recommend anteromedial approach for open reduction[11].
While choosing an approach, one must take into consideration surgeon’s experience and the anatomical structures involved. It is known from various studies that fracture union time and rate of approach related complications are similar with various approaches [7,11].
In a study by Aslan and co-authors, clinical and radiographic results of children with Gartland type 3 supracondylar humerus treated with primary open reduction using four different approaches were studied [7]. Fifty eight patients were treated with either anterior, medial, lateral and , posterior approach. Choice of approach was decided by fracture pattern and neurovascular injury. All fractures were fixed with two lateral entry k wires or crossed k wires as per surgeon’s preference. In this series, three quarters of patients were operated within 24 hours since injury. Flynn criteria were used to measure outcomes. The outcome was comparable in all groups.
Ozkoc and co-authors studied 99 patients with supracondylar humerus fracture. In this group, 44 patients were treated with primary open reduction and k wire fixation and 55 were treated with closed reduction and percutaneous pinning. They found that in the open group the average loss of extension was 6 degrees compared to 0.6 degrees in the closed group[2].
Koudstaal and colleagues have reported the use of anterior approach in 26 children [15]. In another study, Ay and co-authors report their experience of using the anterior approach in 61 children [16]. In both these studies, a transverse incision was used in the antecubital fossa. In both studies, excellent results were noted without any significant loss of elbow movement.
In summary, various options are available for performing an open reduction of a supracondylar humerus fracture. The anterior approach certainly offers advantages of direct visualisation and retraction of entrapped structures. The treating surgeon must choose the appropriate approach based on the indication for open reduction.
Author’s preferred treatment
Our indications for open reduction are as follows:
1) Vascular compromise or disappearance of pulse after doing closed reduction- In this scenario, we suspect the brachial artery likely to be caught between fracture fragments. Hence, we perform an exploration via the anterolateral or anteromedial approach. The vascular structures are explored and reduction of fragments is achieved under vision. We undertake this approach with a vascular/plastic surgeon available in the operation theatre in case the need for vascular repair arises.
2) Inability to achieve satisfactory reduction by closed method- Usually this is encountered in late presentation of fractures with severely swollen elbow. Usually, attempts of closed reduction are made and if satisfactory reduction cannot be achieved, then open reduction is performed. Our preferred approach for this type is usually the anterior approach. However when skin conditions do not permit anterior approach, then a medial and/or lateral approach depending upon the fracture configuration is used.
Open fractures: Usually there is an anterior wound. Anterior approach is used in these cases.
References
1. Mulpuri K, Wilkins K. The treatment of displaced supracondylar humerus fractures: evidence based guideline. J Pediatr Orthop 2012;32:S143-S152
2. Ozkoc G, Gone U, Kayaalp A, Teker K, Peker TT. Displaced supracondylar humeral fractures in children: open reduction vs. closed reduction and pinning. Arch Orthop Trauma Surg 2004; 124:547-551.
3. Cramer KE, Devito DP, Green NE. Comparison of closed reduction and percutaneous pinning versus open reduction and percutaneous pinning in displaced supracondylar fractures of the humerus in children. J Orthop Trauma 1992;6:407-412.
4. Oh CW, Park BC, Kim PT, Park IH, Kyung HS, Ihn JC. Completely displaced supracondylar humerus fractures in children: results of open reduction versus closed reduction. J Orthop Sci 2003;8:137-141
5. Walmsley PJ, Kelly MB, Robb JE, Annan IH, Porter DE. Delay increases the need for open reduction of type –III supracondylar fractures of the humerus. J Bone Joint Surg Br 2006;88:528-530.
6. Mulhall KJ, Abuzakuk T, Curtin W, O;Sullivan M. Displaced supracondylar fractures of the humerus in children. Int Orthop 2000;24:221-223.
7. Aslan A, Konya MN, Ozdemir A, Yougancigil H, Maralcan G, Uysal E. Open reduction and pinning for the treatment of Gartland extension type III supracondylar humeral fractures in children. Strat Trauma Limb Recon 2014;9:79-88.
8. Aktekin CN, Toprak A, Ozturk AM, Altay M, Ozkurt B, Tabak AY. Open reduction via posterior triceps sparing approach in comparison with closed treatment of posteromedial displaced Gartland type III supracondylar humerus fractures. J Pediatr Orthop B 2008;17:171-178.
9. Gupta N, Kay RM, Leitch K, Femino JD, Tolo VT, Skaggs DL. Effect of surgical delay in perioperative complications and need for open reduction in supracondylar humerus fractures in children. J Pediatr Orthop 2004;24:245-248.
10. Reitman RD, Waters P, Millis M. Open reduction and internal fixation for supracondylar humerus fractures in children. J Pediatr Orthop 2001;21:157-161.
11. Mazzini JP, Martin JR, Esteban EMA. Surgical approaches for open reduction and pinning in severely displaced supracondylar humerus fractures in children: a systematic review. J Child Orthop 2010;4:143-152.
12. Fleiriau-Chateau P, McIntyre W, Letts WM. An analysis of open reduction of irreducible supracondylar fractures of the humerus in children. Can J Surg 1998;41(2):112-118.
13. Gruber MA, Hudson OC. Supracondylar fracture of the humerus in childhood. End results study of open reduction. J Bone Joint Surg Am 1964;46:1245-1252.
14. Sibly TF, Briggs PJ, Gibson MJ. Supracondylar fractures of the humerus in childhood: Range of movements following the posterior approach to open reduction. Injury 1991;22(6):456-458.
15. Koudstaal MJ, De Ridder VA, De Lange S, et al. Pediatric supracondylar humerus fractures: The anterior approach. J Orthop Trauma 2002;16(6):409-412.
16. Ay S, Akinnci M, Kamiloglu S, Ercetin O. Open reduction of displaced pediatric supracondylar humeral fracture through the anterior cubital approach. J Pediatr Orthop 2005;25:149-153 .
(Abstract) (Full Text HTML) (Download PDF)
Editorial
Vol 1 | Issue 1 | July – Sep 2015 | page: 1 | Sandeep Patwardhan, Taral Nagda.
Authors: Dr. Sandeep Patwardhan[1], Dr.Taral Nagda[2].
Dr. Sandeep Patwardhan: Paediatric Orthopaedic Surgeon, Sancheti Institute for Orthopaedics and Rehabilitation. Pune, India: Email: sandappa@gmail.com
Dr. Taral Nagda: Paediatric Orthoapedic Surgeon, Institute for Paediatric Orthopaedic Disorders, Mumbai and Jupiter Hospital, Thane, India. Email:taralnagda@gmail.com
Editorial
Paediatric orthopaedics is evolving by leaps and bounds on a day to day basis as we have more insights in to biology and access to improved imaging and technology for management. With the changing demographics of the world, India is poised on the crossroads where we have a healthy mix of educated urban literate population who demands the best management at par with the western world. At the same time we have a large volume of children who are subjected to gross neglect due to inability to access healthcare or poor understanding & quality of training in the country with respect to paediatric orthopaedics. There are only about 50- 60 paediatric orthopaedic surgeons for a population of 450 million children. As we march towards improving paediatric orthopaedic services through improved training acquired through western world, we realised the shortcomings of this training with respect to differential needs of our native populations. No amount of literature or fellowship training in the west can prepare us for management of neglected and complicated paediatric orthopaedic conditions. We realised that we will have to evolve our own strategies and share the knowledge through publications for effective management of our children. We found the existing journals restrictive and difficult to access with respect to their norms of publications. Hence the International Journal of Paediatric Orthopaedics (IJPO) which is an attempt to allow easy open access online sharing of knowledge with emphasis to the eastern world and the different requirements of our populations. I am sure that contributions to this journal will foster a better understanding as well as interactions between the western and eastern worlds. We believe we have a spectrum of disease which is unseen and under-reported in current literature but which is still quite relevant to two thirds of the world. IJPO will aim to provide a platform where global interactions are possible and views and opinions can be shared easily. New formats of articles will be encouraged and in the first issue we have an article written in dialectic format and another in case based format along with the usual review formats. We would welcome articles from all over the world and we hope to be able to make it a patient driven Journal along with being evidence based.
We would like to thank the Orthopaedic Research Group and ResearchOne® Publishers in helping us through the process. We would thank our affiliate body ‘International Fractures in Children Symposium’ (I-FICS) for their unconditional support an allowing the launch of the Journal in their annual meeting. We would like to thank every author who has contributed to the first issue and special thanks to all the editorial board members who have shown faith in us and have joined us in an effort to create a world class journal
Sandeep Patwardhan & Taral Nagda
(Abstract) (Full Text HTML) (Download PDF)
The Effect of Guided Growth on Rotational Deformities of the Long Bones: A Biomechanical Study on Sawbone
Vol 1 | Issue 1 | July-Sep 2015 | page:44-47 | Emre Cullu, Mutlu Cobanoglu, Mustafa Kemal Peker.
Authors : Emre Cullu[1], Mutlu Cobanoglu[2*], Mustafa Kemal Peker[3].
[1] Adnan Menderes University Medical School, Deparment of Orthopaedics and Traumatology,
Turkey.
Address of Correspondence
Dr. Mutlu Cobanoglu
Adnan Menderes University Medical School, Department of Orthopaedics and Traumatology, KepezMevkii 09100 Aydın / Turkey
E-mail: drmutlu79@hotmail.com
Abstract
Background: Although temporary hemi-epiphysiodesis is an effective method for correction of frontal and sagittal plane limb deformity in growing children, osteotomy is commonly performed to correct rotational deformities of the long bones. The aim of this report is to improve rotational guided growth with a formula created to calculate the amount of correction.
Methods: A femur sawbone was cut above the trochlear sulcus. Two 8-plates were placed opposite to each other on medial and lateral sides of the cutting line. Three pairs of holes were drilled in three different angles on medial side and lateral side to place two plates on sawbone. The bone was distracted by an intramedullary device. The anteversion angles were measured by computerized tomography. The angles between the femoral axis and the plates were measured on X-ray. A formula was used to calculate the amount of correction.
Results: As the bone was distracted, rotation of the distal part of the cutting line was observed. When the angles between the plates and the long axis of the bone (α) were 50°, 36°, and 26°, the axial rotations were -11.25°, 2.43°, and 7.06° respectively on CT. When the formula was applied, the amounts of corrections were 25.7°, 18.5°, and 13.4° respectively.
Conclusions: This study supports that this technique can be used for correction of rotational deformities of the long bones. It’s said that the wider angle between the plates and the long axis of the bone, the greater rotation. But further experimental studies are required to improve this technique.
Keywords: Rotational guided growth, rotational deformity, temporary epiphysiodesis.
Introduction
There are many options for the correction of angular bone deformities but the standard treatment has been osteotomy. Currently, hemi-epiphysiodesis is considered an effective treatment to correct an axial limb deformity in children [1,2] and Stevens presented a technique using an 8-plate [3]. Although this technique is an effective treatment method for correction of frontal and sagittal plane limb deformities in growing children, osteotomy is still a commonly used surgical technique for rotational deformities of the long bones. In the recent years, it has been thought that a rotational deformity in the horizontal plane of the long bones could be corrected by guided growth and two animal studies, which evaluated guiding rotational growth, were published [4,5]. In this biomechanical study the aim was to improve rotational guided growth with a formula created to calculate the amount of correction. Because of that a sawbone model was designed.
Materials and Methods
One femur foam cortical shell sawbone with a 15 mm diameter canal and 42 cm overall length was used for the model. A left femoral sawbone, two titanium growth 8-plates (Biomet/USA and TST/Turkey), a distractor of an external fixator, a steel spring, a handle of an umbrella were used to construct this model. The sawbone was cut just above the intercondylar sulcus. This cutting line acted as a physeal line. The sawbone was reamed from the fossa priformis with a 12-mm drill for the placement of an intramedullary device to distract the fragments. The sharp ends of the distractor were cut. The distractor, the handle of the umbrella, and the spring were placed into the medullary canal via fossa priformis and fixed with glue gun. The outer part of the handle was cut and used as an antirotation block in the canal. The block was glued to the sawbone through a window opened from posterior surface of the proximal side of the cutting line. This block prevented the rotation of the distractor in the canal. The tip of the spring was fixed with glu to the distal fragment. This spring was placed between proximal and distal fragments. When the device was distracted, the device pushed the spring toward the distal fragment. By this way the lengthening was obtained. Because of the spring, distractor did not create an external rotation force on the distal fragment by itself directly (Figure 1).
Three pairs of holes were drilled in three different angles to place plates on the sawbone, Two 8-plates, whose brands were different, with four screws were used to fix the cutting line and were placed on medial and lateral side of the bone (Fig 2). The different plates of different brands were helpful to differentiate one plate from the other on lateral X-ray. To create external rotation the medial plate was placed obliquely from the proximal anterior region to the distal posterior region, and the lateral plate was placed obliquely from the proximal posterior region to the distal anterior region (Figure 3).
Fixation of the plates was performed in three different angles. The screws were not tightened completely. An allen wrench was used to distract the intramedullary device on its proximal end. The distances between proximal and distal holes were measured in each plate manually. The angles between the femoral axis and the plates were measured on lateral X-ray. Femoral length (FL) (from the tip of trochanter major to top of intercondylar notch), mechanical lateral distal femoral angle (mLDFA), anatomic posterior distal femoral angle (aPFDA) were evaluated on computerized tomography (CT) scanogram. The femoral anteversion of the sawbone was measured on CT. A flat surface was used to immobilize the sawbone and to standardize the evaluation of the rotation. Retroversion was defined as negative value, anteversion was defined as positive value. All parameters were evaluated on PACS (Picture Archiving and Communication System) radiologic system. A formula was created to calculate that how many degrees the plates should be placed to obtain desired amount of rotation. Depending on the length and angle of the plates, the arc length scanned by the plate was equal to the arc length scanned by the distal fragment until the plate became horizontally. Additionally, the arc length scanned by the distal fragment depended on its radius. The length of the arc (the distance between the first position (B) and the last position (B’) of the distal screw of the medial plate) swept by the plate is equal to the path drawn by the rotation around its axis of the distal region (Figure 4).
The virtually spiral movement of this region along the axis is shown as the progress of the arc on the surface of the cylinder (Figure 5). A full rotation of the arc of the helix is equal to the diagonal line of the open shape of the cylinder.
The formula which was created to calculate the amount of correction (θ) is demontrated as follows:
BB’ 2Π·ΑΒ·α/360
KK’ 2Π· MK·θ/360
BB’KK’
2Π·ΑΒ·α/360 2Π·MK·θ/360
θ ΑΒ·α /MK
(A: Position of the proximal screw of the medial plate, B: The first position of the distal screw of the medial plate, B’: The last position of the distal screw of the medial plate, α: The angle between long axis of the sawbone and medial plate, M: Center of the distal region of the bone. K: Starting point of the rotation. K’: End point of the rotation. MK=MK’: Radius of the distal region of the bone. θ: Rotation angle)
Results
The FL was 421.79 mm and the anteversion of the sawbone was 8.26° before distraction. When the sawbone was distracted, rotation of the distal fragment was observed without translation (Figure 6). When the angles between the plates and the long axis of the bone (α) were 50°, 36°, and 26°, the axial rotations were -11.25°, 2.43°, and 7.06° respectively on CT and the FLs were 433.38mm, 430.02mm, 429.74mm respectively after full distraction. Thus, the amount of correction (θ) were 19.25°, 5.83°, and 1.20°, respectively. The wider the angle between the plates and the long axis of the bone, the more rotation and lengthening occurred. As the screws were not tightened completely, rotation of the plates, which led to more rotation of the distal fragment and lengthening of the bone, occurred more easily.
In the coronal plane, mLDFA was 87° before lengthening. After lengthening mLDFAs were constant when the α angle were 50° and 36°. But mLDFA was 83° when the α was 26°.
In the sagittal plane, aPDFA was 89° before lengthening. After lengthening aPDFAs were 90° when the α angles were 50° and 36° and aPDFA was 91° when the α angle was 26°.
The distance between the screw holes (AB) was 18 mm, and the radius of the distal fragment of the femur (MK) was 35 mm. When the formula was used, the amounts of correction (θ) were 25.7°, 18.5°, and 13.4°, respectively. None of the calculated degrees of correction were comparable to the CT measurements.
Discussion
Angular deformities around the knee can be corrected with hemiepiphysiodeses in skeletally immature patients [2,6,7]. The epiphysis grows symmetrically under normal conditions. If the physeal plate is compressed from one side, an angular deformity can occur. Mechanical modulation of longitudinal growth by compressive forces is a widely accepted notion, also known as the Volkmann’s law [8]. However, osteotomy is the most commonly used surgical technique for the correction of rotational deformities of the long bones. Furthermore, rotational guided growth are not currently used to correct rotational deformities of the long bones in clinical practise. There are two reported animal studies [4,5]. Arami et al used rabbit femur in their study and to induce external rotation the distal part of the medial plate was positioned posteriorly and to induce internal rotation the distal part of the medial plate was positioned anteriorly. They said that because of the shape of the medial femoral condyle, some technical difficulties occurred and medial plate was placed in desired position in the group of external rotation [4]. The physeal line of the distal femur of rabbit is wavy and not straight. For this reason to place both plates obliquely in different directions on wavy line is not seen feasible. Firstly more straight physeal line is needed. Cobanoglu et al studied on the proximal tibial epiphysis of rabbit to induce external rotation. The reason why they preferred proximal tibia to distal femur could be that the proximal tibia had straighter physeal line than distal femur. They only studied on external rotation group and did not create a formula about prediction amount of rotation [5]. This study is a biomechanical study. And the aim of this study is to create a formula based on the angle between the long axis of the bone and the plates. A distal femoral physeal plate was created by cutting the sawbone just above the trochlear sulcus and two 8-plates were placed on either side of the cutting line. It was thought that if two plates were placed at reverse angles to each other on either side of the bone, the distal fragment would be rotated. According to this theory, the screws in the holes should not be tightened completely to create rotation points or free zones between the plates and screws. These rotation points would cause the plates to spin around the screws like a hinge. The screws were placed as closely as possible to the cutting line, and thus the plate placement angle was increased. We used an intramedullary device to distract the bone. While the sawbone was being distracted, rotation of the distal fragment was obtained and this led to a reduction in the anteversion of the femur due to the placement of the plates. The upper limit of rotation which can be corrected, is due to orientation of the plates and the distance between the proximal and the distal screws. Therefore, insertion of these plates with the greatest angle to the long axis as possible and the greatest distance between the screws as possible will lead greater rotation. These are two important variables in the formula. These variables are related to anatomical properties of the bone such as width and points for plate fixation. The angle between the positions of the plate and the bone axis needs monitoring. For this reason, the position of the plates at the end of the rotational correction is crucial to prevent angular deformities. The important points of this technique are the distance between the proximal and distal screws and the tightness of the screws. The use of long plates results in greater lengthening and rotation, depending on the distance between the holes. When the distance between the proximal and distal screws is as great as possible, increased gap between the fragments and more rotation of the distal fragment are observed. And to be able to obtain rotation of the plate more easily, the screws must not be tightened completely. Another important point is that placement of the plates at the same angle onto the bone. For this reason, the amount of rotation will reveal according to the plate having less angle with bone axis. When the axis of this plate is parallel to the bone axis, the plate will not rotate and causes a deformity. So the deformities of the condyles can affect the rotational measure. Arami et al used inter-plate angle in their study and declared that every 1° of change in this angle corresponded 0.378° of rotational profile difference [4]. In our opinion because of the reasons mentioned above, the rotational profile is dependent on the angle between the plate and bone axis, not inter-plate angle. The CT measurements and calculations using the formula differed from each other. There are three possible reasons for this disparity: First, there was laxity between the screws and the plates, leading to instability between the proximal and distal regions of the sawbone. Second, the sawbone had a circular structure whereas the plates were straight. These incompatible shapes might prevent rotation. Third, the distal region of the bone does not form a precise circle. This technique has not been performed to humans yet. This biomechanical study supports that this technique can be used for the correction of rotational deformities of the long bones. It’s said that the wider angle between the plates and the long axis of the bone, the greater rotation. But further animal studies are required to demonstrate efficacy of this hypothesis.
References
1. Houshian S, Mehdi B, Larsen MS. The epidemiology of elbow fracture in children: analysis of 355 fractures, with special reference to supracondylar humerus fractures. J Orthop Sci 2001;6(4):312-5
2. Barr LV. Pediatric supracondylar humeral fractures: epidemiology, mechanisms and incidence during school holidays. J Child Orthop. 2014; 8:167–170
3. Cheng, Jack CY, Ng, BKW, Ying, S. Y, Phil P. A 10-Year Study of the Changes in the Pattern and Treatment of 6,493 Fractures. 19(3), May/June 1999, pp 344-350
4. Kemp AM, Dunstan F, Harrison S, Morris S, Mann M, Rolfe K, Datta S, Thomas DP, Sibert JR, Maguire S. Patterns of skeletal fractures in child abuse: systematic review. BMJ 2008; 337:a1518
5. Strait RT, Siegel RM, Shapiro RA. Humeral fractures without obvious etiologies in children less than 3 years of age: when is it abuse? Pediatrics. 1995 Oct;96(4 Pt 1):667-71
6. Cheng JC, Lam TP, Maffulli N. Epidemiological features of supracondylar fractures of the humerus in Chinese children. J Pediatr Orthop B 2001;10(1):63-67
7. Mahan SD, May CD, Kocher MS. Operative Management of Displaced Flexion Supracondylar Humerus Fractures in Children. J Pediatr Orthop 2007;27:551-556
8. Leitch KK, Kay RM, Femino JD, Tolo VT, Storer SK, Skaggs DL. Treatment of multidirectionally unstable supracondylar humeral fractures in children. A modified Gartland type-IV fracture. J Bone Joint Surg Am. 2006 May;88(5):980-5.
9. Skaggs DL, Flynn JM. (2010) In Rockwood and Wilkins’ Fractures in Children. Philadelphia. Lippincott Williams and Wilkins. 514-515
10. Bahk MS, Srikumaran U, Ain MC, Erkula G, Leet AI, Sargent MC, Sponseller PD. Patterns of Pediatric Supracondylar Humerus Fractures. J Pediatr Orthop 2008;28:493-499.
11. Sen RK, Tripathy SK, Kumar A, Agarwal A, Aggarwal S, Dhatt S. Metaphyseo-diaphyseal junction fracture of distal humerus in children. J Pediatr Orthop B 2012, 21:109–114
12. Blount WP. Fractures in Children. Baltimore: Williams and Wilkins, 1955
13. France J, Strong M. Deformity and function in supracondylar fractures of the humerus in children variously treated by closed reduction and splinting, traction and percutaneous pinning. J Pediatr Orthop. 1992:12(4): 494-498
14. Khoshbin A, Leroux T, Wasserstein D, Wolfstadt J, Law PW, Mahomed N, Wright JG. The epidemiology of paediatric supracondylar fracture fixation: A population-based study. Injury. 2014; 45: 701–708Khoshbin A, Leroux T, Wasserstein D, Wolfstadt J, Law PW, Mahomed N, Wright JG. The epidemiology of paediatric supracondylar fracture fixation: A population-based study. Injury. 2014; 45: 701–708
15. Kasser JR. Location of treatment of supracondylar fractures of the humerus in children. Clin Orthop Relat Res. 2005 May;(434):110-3
16. Slobogean BL, Jackman H, Tennant S, Slobogean GP, Mulpuri K. Iatrogenic ulnar nerve injury after the surgical treatment of displaced supracondylar fractures of the humerus: number needed to harm, a systematic review. J Pediatr Orthop 2010;30(5):430-6
17. Lyons, James P. M.D.; Ashley, Edwin M.D.; Hoffer, M. Mark M.D. Ulnar Nerve Palsies After Percutaneous Cross-Pinning of Supracondylar Fractures in Children’s Elbows. J Pediatr Orthop. 1998:18, 43-45
18. Lee YH, Lee SK, Kim BS, Chung MS, Baek GH, Gong HS, Lee JK. Three Lateral Divergent or Parallel Pin Fixations for the Treatment of Displaced Supracondylar Humerus Fractures in Children. J Pediatr Orthop 2008;28:417-422
19. Kocher MS1, Kasser JR, Waters PM, Bae D, Snyder BD, Hresko MT, Hedequist D, Karlin L, Kim YJ, Murray MM, Millis MB, Emans JB, Dichtel L, Matheney T, Lee BM. Lateral entry compared with medial and lateral entry pin fixation for completely displaced supracondylar humeral fractures in children. A randomized clinical trial. J Bone Joint Surg 2007;89(4):706-12
20. Mahan ST, Osborn E, Bae DS, Waters PM, Kasser JR, Kocher MS, Snyder BD, Hresko MT. Changing Practice Patterns: The Impact of a Randomized Clinical Trial on Surgeons Preference for Treatment of Type 3 Supracondylar Humerus Fractures. J Pediatr Orthop 2012;32:340–345
21. Battaglia TC, Armstrong DG, Schwend RM. Factors affecting forearm compartment pressures in children with supracondylar fracture of the humerus. J Pediatr Orthop. 2002; 22(4): 431-439
22. Blackmore LC, Cooperman DR, Thompson GH. Compartment syndrome in ipsilateral humerus and forearm fractures in children. Clin Orthop and Relat Res. 2000; 376: 32-38
23. Campbell CC, Waters PM, Emams JB, Kasser JR, Millis MB. Neurovascular injury and displacement in type 3 supracondylar humerus fractures. J Pediatr Orthop. 1995;15(1):47-52
24. Choi PD, Melikian R. Skaggs DL. Risk Factors for vascular repair and compartment syndrome in the pulseless supracondylar humerus fracture in children. J Pediatr Orthop 2010;30:50-56 .
(Abstract) (Full Text HTML) (Download PDF)